As things change, and change rapidly, I wanted to continue reaching out to you with regards to COVID-19 (what you may also know as the coronavirus). There is a lot of information out there, so allow me to help digest and interpret it with you.
So, in this article, I want to detail what we know, what’s changing, and what action steps might be best for your health right now. Personally, I believe we are at a different point than even a week ago when it comes to the projections, our focuses, and our strategies.
All that in mind, it’s time to update those and what they mean for you. Let’s get started.
A Summary of What’s Ahead
Current projects suggest that we are going to see the vast majority of Americans develop COVID-19 throughout the course of the year. Hopefully, it won’t be you, but odds are that it will be given where we currently stand.
Given that, what are the best things you can do to cut your risk for complications? That is for you, as well as for those you are currently sheltering in place along with you.
How Did We Get To This Point?
Every day, I have been spending a fair amount of time reading the latest medical literature surrounding this pandemic and what it means.
What I have learned is that things are happening so fast, it’s almost as though things are changing on a minute-to-minute basis. Research is constantly emerging, and it is shifting our perspective whenever it does.
Seeing some of the newest papers, I started thinking about just what are the real implications coming out of these developments.
The first thought that comes to mind is trying to understand the “peak” of this crisis. When will we see the COVID-19 pandemic crescendo and hit its highest point?
Key Insight: Right now, that date appears to be around April 14th or 15th. While the peak doesn’t mean that it’ll be gone on April 16th, it does mean that the number of new cases and deaths will likely be lower than the day before it (but it does not mean none).
In fact, it is likely going to take quite some time before it ramps down to a lower number, and we will have some lapses afterward, too (which will shift based on regions).
What Can Change The Peak?
The next thing that we need to think about is how to slow that down and how to make it so that the peak itself does not hamper the medical infrastructure of the country.
As I mentioned, it’s more a matter of when, not if, the majority of Americans get infected with COVID-19. Instead, we have to think in terms of timing and how it affects our medical system.
Some of the main considerations for slowing things down have been:
- Antivirals
- Vaccines
- Herd immunity
Let’s touch on all of these…
Antiviral Vaccines
These are the medications which can kill viruses. You can think of them as antibiotics for viruses, things that make them not properly replicate and “kill” them.
What we know is that antibiotics are hard to make, and there is very little cost incentive to go around making more of them.
That’s because, if people need them, they only need them for a short period of time. They are driven by context, and are not something people take daily.
Ultimately, they are medications that have not had much active support or research for that reason. When you think of antiviral medications, these complications are even worse.
We have had a lot of research and development on HIV, which has been great, and it has also expanded our understanding of how viruses respond.
However, it has also shown us that they are not easy to treat. They are even harder to treat than bacteria.
Key Insight: The mean timeframe to get a new medication on the market, specific to antiviral medication, is roughly 6.4 years. Of course, we can be more aggressive and speed that up, but this is the average time to date.
That said, 6.4 years, as aggressive as we might like to be, cannot be turned into only a handful of months. It has to come in incremental gains.
We may learn more about the existing medications currently in use, but an antiviral in time for the end of 2020 is unfeasible.
Bottom Line: When we hear about medications that can be taken in combination, many of these currently being talked about bringing cardiac issues with them. This is especially relevant because one of the ways COVID-19 causes mortality is by causing cardiomyopathy.
Medications may be a very helpful thing, but it is very likely that we will not see them in the shorterm. And any options we currently have or are being discussed may bring side effects that can cause more harm than good.
Vaccines
What’s the latest data when it comes to COVID-19 vaccines? When we’re talking about this kind of virus, it is quite difficult to make safe vaccines for them.
That is mainly because of the nature of their protein coats, the number of strains that can come about, and the difficulty revolves around getting enough of the antigenic material (the surface coats that identify the virus to your immune system).
You want enough of that to get immunity, but you don’t want so much of that to the point that it makes you sick. With vaccinations, more generally, that’s always the trick — how do we get enough to grant immunity but not so much that you may as well have it.
For this particular category, while it has been achieved more, it is incredibly complex and not easy at all.
The thought is that you could use a certain amount of surface coaters, and that could give you some level of passive immunity, but it may not last with real-world exposure.
Bottom Line: It will likely be a little while before we can safely say that a vaccine for COVID-19 is working. Most experts are projecting years, but aggressive timelines suggest 18-36 months if all goes well.
Herd Immunity
Basically, if enough people have had an illness, they are resistant to it. And, data with respect to COVID-19, has revealed a certain time frame where you are no longer contagious and you likely have some lasting immunity, too.
In the case of measles, for example, if 95% of the population has an immunity to it, it won’t really ever get the chance to take root in that particular population. There simply aren’t enough susceptible people to pass it around with great effect.
Even if some got it in isolated cases, it simply wouldn’t be able to make its way around and throughout the population.
Specific to COVID-19, that would require 60-70% herd immunity. That much exposure would be required to where, overall, the risk cannot take off like the wildfire we are currently seeing.
So, how long would something like that take? That is very likely to occur in 10-12 months from now. That is worth underscoring and thinking through.
Key Insight: By the time 2020 is over, we think that 60-70% of Americans will have had COVID-19. That means a lot of people will be sick, but will result in some passive immunity.
What About Mortality Rates?
This is something we need to think through. We currently have data from China and South Korea suggesting that the mortality rate may be falling somewhere in between 0.1% – 0.4%.
That said, many experts believe that the rate will be quite different in the United States. That’s because mortality is highly correlated to certain risk factors at play.
This would include:
- Age
- Blood Pressure
- Kidney Function
- Smoking Status
- Obesity
Most of those who died, in China, were men over the age of 70. Turns out, though, that Chinese men over the age of 70 almost all smoke (around 70% or more). Compared to Chinese women in this same age group, less than 9% of them smoke.
So, was it really just the age or more so the smoking status that had an effect? In addition, in the United States, we have less total smokers but a higher rate of those who are dealing with obesity (relative to China).
When we think these things through, what do they mean? If you run the numbers, you’re likely to see estimates in the 1.5% range of mortality rate. That’s because we have many more people who fit those aforementioned risk factors.
Bottom Line: Over the course of this coming year, that may look like approximately 2.9 million deaths. We hear a lot about 100,000 being a great goal, but that’s simply for the current surge.
What Does This All Mean For Your True Risk?
When we think about herd immunity, exposure, and mortality rates, what do all of these factors combined mean for your health?
Well, all you really have to do is flip a coin.
If you toss a coin and get heads, you don’t have it. But, you have to toss it again. At some point, you are eventually going to get tails and get COVID-19. It’s more a matter of when.
When Is The Best Time To Get It?
If we shift our perspective to the inevitability of getting COVID-19, when is the best time to get it? Should we look to get it sooner, or later, and how do our chances of surviving fluctuate were we to get it.
I have seen some people argue that there may be an advantage to getting it earlier, because there are a lot of supply chain issues that have not fully manifested. Not simply masks or ventilators, but the common medications used in ICU care.
In the coming days and weeks, we may see a shortage of these things which is going to make contracting COVID-19 all the more difficult for patients. That’s where this argument for getting it sooner is born.
On the other hand, the overall net effect of getting it later is likely the better option. This is based around three principal theories:
- It’s better for society
- Puts less burden on hospitals
- We learn more about treatment
Bottom Line: Getting it later also means that we may reach herd immunity before your risk of getting exposed ever comes around. I would strongly argue against getting early exposure.
The Implications of Physical Isolation
I am really glad that we have decided to focus on the term “physical isolation,” rather than “social isolation.” Because, really, you don’t want to socially isolate yourself at all.
You want to keep your mind active, your body moving (and exposure to the outdoors whenever possible), but to really be conscious of your presence and your presence around others.
All it takes is thought and planning. You want to be cognisant of where you can go, without people around, and how you can catch a breath without finding yourself in a crowd.
Bottom Line: As much as you can, be conscious of everything and clean as much as possible. Wash your hands, packages, try not to touch buttons with your fingers (like on an elevator), and keep inside as often as your lifestyle allows.
Having said that, there will still be many people who do all the right things and still catch COVID-19. These are guidelines, but they are not a guarantee.
So, if you are doing some version of sheltering in stay, can you do a solo quarantine (or what we might call self-isolation)?
I imagine that there are a lot of people out there who, if they got infected, would be unable to use a guest home or afford other lodgings to stay away from their family or those they live with, it just wouldn’t be possible.
In most cases, if you are exposed and you get COVID-19 you are very likely to give it to someone who lives with you or close to you. Going into this, then, we need to start thinking about the most vulnerable members of our family.
So, what can you do to ensure you don’t get any complications? First, it starts by understanding what those complications might be in the first place.
Who Is Prone To Hospitalization and Complications?

Let’s start by breaking down the various categories that may be most at risk…
Renal Disease
The first one I want to discuss is renal disease. I’m talking about it first because it is one of the more manageable issues at hand.
Around 15% of the population may have renal disease, whether or not they know it, and around 80% of it is undiagnosed.
The main thing you can do to help with it is improving your blood sugar, and improving your blood pressure. Those are things we’ll come back to, but they are prevalent here.
Age
Next, we need to think about age. It’s obviously not one we can change, but one thing to note is the fact that the data is currently skewed.
While many Chinese youth had little issue with COVID-19, many more American youth have issues with obesity which could lead to much worse results.
Obesity
Building on that, let’s discuss obesity and what it may mean.
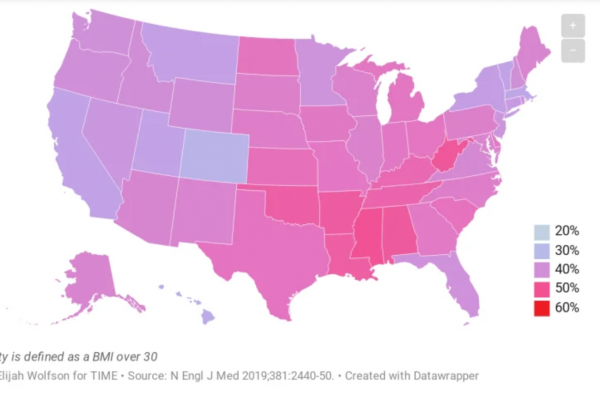
Per state, the average obesity rate falls somewhere around 40%. This varies, state by state, but this is likely a fair average nationwide.
I have discussed before what all this means, and how obesity is a disease and not simply a label for a person who fits into certain measurements.
What we have seen in terms of the additional risks is that it is not simply height to weight, it is more the growth of fat in and around the organs themselves.
That is best translated with height-to-waist circumference. As it stands, our knowledge around COVID-19 revolves around height-to-weight.
Specifically, it is based upon body mass index (BMI). The chart below is instructive, because it can help you determine where you fall on the scale.
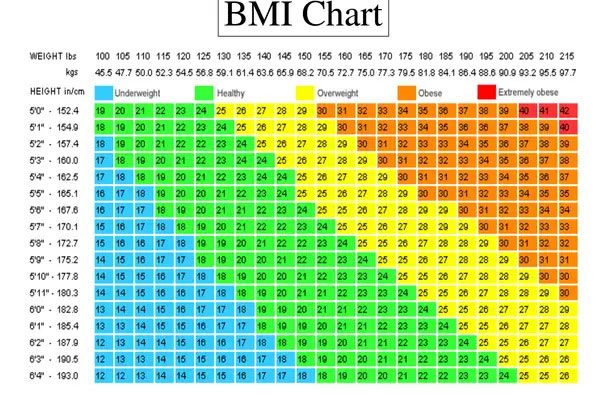
We define obesity as a BMI of 30 or higher, and overweight as 25-30. We now have more detailed versions of mild, moderate, and severe obesity, which replaced older terms.
Do know, though, where you sit on that continuum and what it could mean for your health. We’ll dive a bit deeper into that later on.
Bottom Line: This whole pandemic is leading to a lot of stress and a lot of “comfort eating” to help us stay calm. That’s totally understandable, but we do need to understand the risks that come along with that.
Chronic Pulmonary Disease
The prevalence of this is around 16 million Americans with some sort of mixture of chronic obstructive pulmonary disease, chronic bronchitis, or emphysema.
So, what can you do about that? The first is to stop smoking and quitting smoking. Vaping is also very popular now, but what we know is that it is certainly not safer than smoking.
Another risk factor, as part of this, is particulate exposure in the air around us (indoor air quality). And then exercise, and how much lung reserve we have because of our fitness.
Blood Pressure
We define hypertension as blood pressure levels which are consistently greater than 130/80. This is extremely prevalent, as this can be a third of the majority of Americans (depending on the demographics in question).
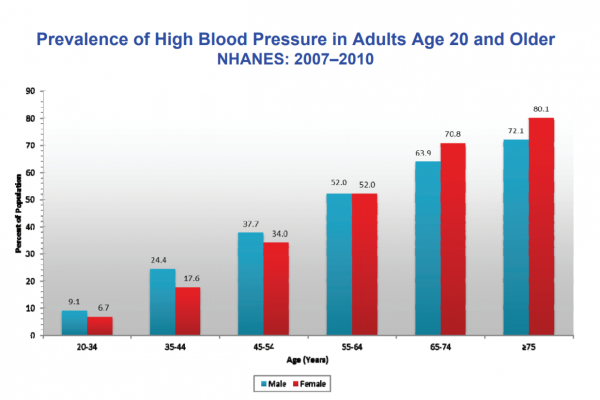
There are also differences per ethnicity which can be a factor.
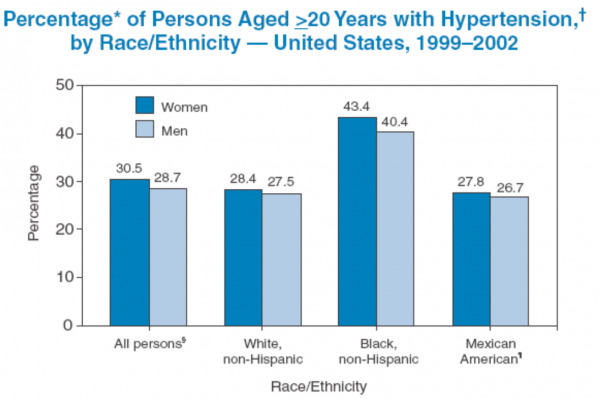
So, ultimately, this is a lot of people and a big direct risk factor for complications and greater tendencies toward kidney disease (which is a secondary factor).
Diabetes
This is quite relevant, so let’s break it down by types (Read More: How To Prevent Diabetes with an Underactive Thyroid).
Starting with Type 1, this is generally younger people and significant because COVID-19 complications are prevalent in the young with Type 1 diabetes (and adults with Type 2).
We define diabetes based upon blood sugar levels. So, we look at your short-term blood sugar (your morning fasting glucose), and your three-month approximation of glucose (A1C).
Those who are at risk are those who have a morning fasting glucose somewhere above 89 (this is one of our current best estimates) and an A1C of about 5.4.
With those who have out and out diabetes, they have a fasting glucose of 125 at all occasions, or they have an A1C of 6.4. That is pretty common stuff.
Key Insight: If we combine those who have diabetes, and those who are at risk of developing it, that’s the majority of Americans in the entire country.
One of the biggest predictors of diabetes in a population is how often that population walks or bicycles from place to place (as a means of transportation).
America doesn’t do much of that. Most of the time, people will drive to get around. That is a big relevant risk factor when you tie the two together (and will likely only get worse).
Implications and Action Steps
So, given everything that we discussed today, it is likely that you will get COVID-19. The odds are against you, and that’s just a fact. It’s not a guarantee, and I truly hope you won’t, but these are the facts before us right now.
Key Insight: If you end up avoiding it, and we reach a point of herd immunity before you get it, that’s awesome. In fact, that’s the very best-case scenario.
But, what if you do get it? What can you do and what action steps should you take?
It’s not just about you, either, it’s about those that you are close with and those you are sharing space with during this time.
As it stands the biggest risks to your health were you do get COVID-19 would be your:
- Body mass index
- Blood pressure
- Blood sugar
It can only be a win for your health if you improve upon these key things. If not for COVID-19, but for everything else in your life (and for the people around you).
Bottom Line: In some ways, we are what we do and we are who we are within. So, together, as a family or as a group, this is a great opportunity to improve your life, your health, and your chances of getting through this pandemic successfully.
Action Steps You Can Take Today
In general, you want to get fit.
You want to move, you want to become lean, and you want to become healthy as a result. When you do this, you end up making key improvements to some of the most common risk factors, including:
- Obesity
- Blood Pressure
- Diabetes/Diabetes Risk
- Lung Health
- Weakened Immunity
- Chronic Stress
- Insomnia
What’s the best way to do that, then? How can we work to drop visceral fat and not regain it to put ourselves in pole position to succeed?
Well, that was one of the main questions I had when I was putting together the Metabolism Reset Diet.
Perhaps you have cut some things out, moved more, and lost a sizable portion of weight (and kept it off). That is awesome, but for a lot of people it doesn’t work that way.
Instead, things either don’t work at all or they relapse quickly. After hearing so many of those stories, I went through all the medical literature and realized some of the key variables:
- Adequate Protein
- Appetite Control
- Length of Adjusting Food Intake
This made me consider a process whereby you could maintain or reset your diet, by quarter, to help eliminate the yo-yo dieting of the past and keep your appetite in check.
A big part of it is your liver, and why you need nutrients to help support it. This, in addition to a premium on protein, vegetables, and resistant starch (Read More: The Full Story On Resistant Starch) results in a winning combination.
You want to include a lot of food diversity, lots of good plant foods, and lean protein. Then, you need to maintain a simple regimen for making it effective to eat less and not relapse.
That’s what meal replacement is all about. All you need to do is trust easy, pre-made liquid meals to help handle your hunger while getting all the same nutrients.
Key Insight: When it comes to snacking, you should always embrace unlimited foods. Vegetables you can munch on during the day to help your hunger.
That’s the basic idea behind the Metabolism Reset Diet, and it’s the best approach that I have found to help people to improve their waist and BMI (while keeping it off).
Bottom Line: If your BMI is not where you want it to be, I would encourage the Metabolism Reset Diet. It really is your best start to help get your health in order.
At-Home Action Steps
If you are not on an active reset, what can you do for maintenance during these times?
The single biggest thing that I would encourage is movement. And, it all starts with the steps, which may just be the hardest thing to get these days.
Ideally, you don’t want to train hard, but you do want to move. That looks like 12,500 steps per day. A pedometer is a great place to start, or your phone/watch. All you have to do is find a way to count your steps.
How do you get more steps during quarantine, here are some ideas:
- Step ups around the house (on your staircase)
- Pacing around your home (like a light walk)
- Going outdoors while practicing social distance
What About For Your Children?
At this point, your children are likely at home and not really sure what to do with themselves. They now have a lot of free time, and not much to do with it.
The biggest thing that you can do is focus on food quality and movement. Above the age of 6, you should try and help them get 10,000-12,000 steps every day (as a minimum).
At the same time, increase their water, produce, fiber, and lean protein. In fact, I have found that shakes are truly a great breakfast for the entire family!
When Should You Do A Reset?
It will all depend on your BMI.
While time will likely show that body fat or height-to-waist ratio is more sensitive to COVID-19 complications, BMI is the best that we have for the time being.
That said, if yours above is 25, please try the Metabolism Reset Diet once per quarter. When 25 and under, please try it once per year.
Ready To Reset?
You’re in luck, because we have a free challenge starting on April 13th.
This is going to be specifically tailored to those who are currently sheltering, quarantining, or self-isolating, to help them reset without worry.
Basically, if your BMI, blood pressure, or blood sugar are not ideal right now, I hope you will consider joining me. I think it will leave a great impact.
As always, I hope you are staying safe, staying well, and please consider everything we talked about today. The situation around COVID-19 is always changing, and I will be here to touch base with you real soon if anything changes.
Until then, I wish you, your family, and all of your loved ones the best in these uncertain times.
1. Schedule a Thyroid Second Opinion with me, Dr. C, Click Here for Details
2. Download and use my Favorite Recipes Cookbook Here
3. Check out my podcast Medical Myths, Legends, and Fairytales Here
Dr. Alan Glen Christianson (Dr. C) is a Naturopathic Endocrinologist and the author of The NY Times bestselling Adrenal Reset Diet, The Metabolism Reset Diet and The Thyroid Reset Diet.
Dr. C’s gift for figuring out what really works has helped hundreds of thousands of people reverse thyroid disease, lose weight, diabetes, and regain energy. Learn more about the surprising story that started his quest.


