Let’s talk about the mechanisms by which we know it works, the evidence we have from studies of populations, and also some evidence we have from interventional trials. All of these line up to give us a really comprehensive overview of how iodine causes thyroid disease.
In fact, concerns about iodine factored heavily into creating my Ultimate Hypothyroid Bundle (Click Here: Learn more about this bundle today). It’s why everything I put together in there is conscious of iodine for your best health
An Overview On Iodine
To date, iodine is known to be one of the best-documented causes of basically all types of thyroid disease, including:
- Hypothyroidism
- Hyperthyroidism
- Thyroid Cancer
- Autoimmune Thyroid Disease
- Goiter
- Toxic Nodular Goiter (Read More: How to heal nodules naturally)
- Nodules
- Congenital Hypothyroidism
These are all things that can be affected by iodine. And, this can be incredibly relevant in terms of dietary iodine, supplemental iodine, iodine in water, in medications, or even as a contrast. It can, and does, work in all these different ways.
The big takeaway, though, is that I don’t want iodine to look like the “bad guy.” It’s not, because we need it, but there is an incredibly narrow range between how much is going to be right for us — and how much is going to be wrong.
Here’s the exciting part, though: What we’re learning now is that getting to the low end of that range is an opportunity to reverse many kinds of thyroid disease. So, there is most definitely hope and a light at the end of the tunnel if you are suffering.
How Does Iodine Slow The Thyroid Down?
I want to introduce you to something called the “Wolff-Chaikoff” effect. The upshot of it is that the thyroid has this capacity to pull in iodine, and to use it to make thyroid hormone.
The cycle is that iodine becomes attached to a protein, called thyroglobulin, and those elements become pulled apart. What you end up with are T4 and T3, which go into the bloodstream.
So far so good, but when there is a lot of iodine, if there were no regulatory mechanism, the body can make so much extra thyroid hormone that it can be fatal.
That is why we have this protective mechanism, called the “Wolff-Chaikhoff” effect.
Illustrating The Wolff-Chaikoff Effect
Here is an image that should help your understanding of it…
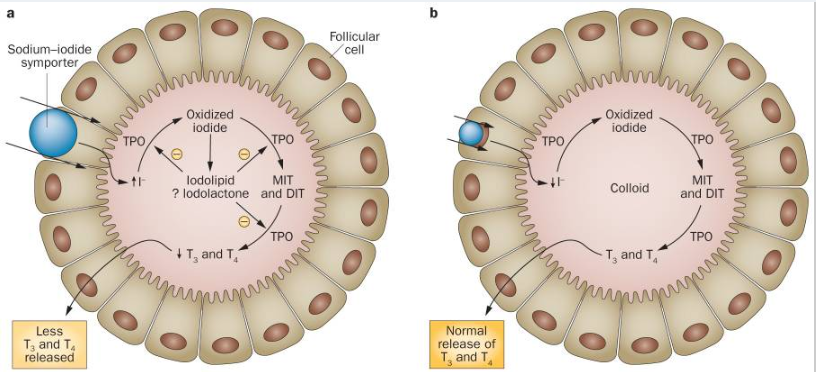
In the case of normal function, on the right, iodine is brought in, the enzyme thyroid peroxidase oxidizes iodide into iodine, and then that is attached by oxidation to thyroglobulin and forms things like T3 and T4 and is released.
On the left is when Wolff-Chaikoff is engaged. What happens is the sodium-iodide symporter is restricted, meaning it is not taking in iodine as well. Because there is such an excess, though, there is still a lot of iodine that has gotten in.
What that means is that you have more that has gotten oxidized iodine, and there are various lipids that are formed. These are free radical compounds, and they damage the effects of thyroperoxidase and make it less able to work.
They also tend to cause thyroglobulin to become more foreign-appearing to the immune system. The net effect, ultimately, is that there is less T3 and T4 released.
Key Insight: Because of all that extra iodine, the mechanisms don’t work as well and everything gets slowed down. Essentially, your thyroid blows a fuse!
All of this is done, though, to be helpful. That’s because if you didn’t slow things down, there would be harm from all that excess that comes out.
This process can come about fairly quickly, and once it’s going on it may last from days to weeks. And, in fact, it may never stop. A common timeframe is about 2-3 weeks for it to come on, but it doesn’t always end.2
We call this the escape phenomena, but some don’t have that happen. We also know that it is not all or nothing — you can have this dramatically shut down your thyroid, or partially slow down your thyroid for longer periods of time.
Breaking Down The Evidence
So, what is the evidence we have for this happening? There was one study done in which it showed that even small amounts of this can be impactful and can be quite harmful.3
In this study, a supplement containing 250 micrograms (mcg) of iodine was given daily to those who had positive thyroid antibodies (but there thyroid function was overall stable) (Read More: How much iodine do you really need?). This meant that they had evidence of Hashimoto’s, but they were not yet in a hypothyroid state.
When this group was given a small amount of iodine, they had nine times the people develop thyroid disease as those did who were not given supplemental iodine. Roughly half of them who developed abnormal thyroid function did not return to normal after stopping iodine supplements.
We know that this works because this is what’s done when someone has too much thyroid hormone being made. There is a condition known as “hyperthyroid storm” which is one of the most dangerous things in all of thyroid disease.
It is a combination of Graves’ disease (Read More: What you need to know about Grave’s disease), where too much thyroid hormone causes the thyroid to make too much hormone. This cycle gets so severe that it can be fatal. People can go into septic shock from having it.
In the moment, the most effective way to stop someone from it is to give them a huge dose of iodine. This thereby forces the Wolff-Chaikoff effect to take place.
How Does Iodine “Turn On” The Immune System?
I want to share another image, which you can see below, to make my point here…
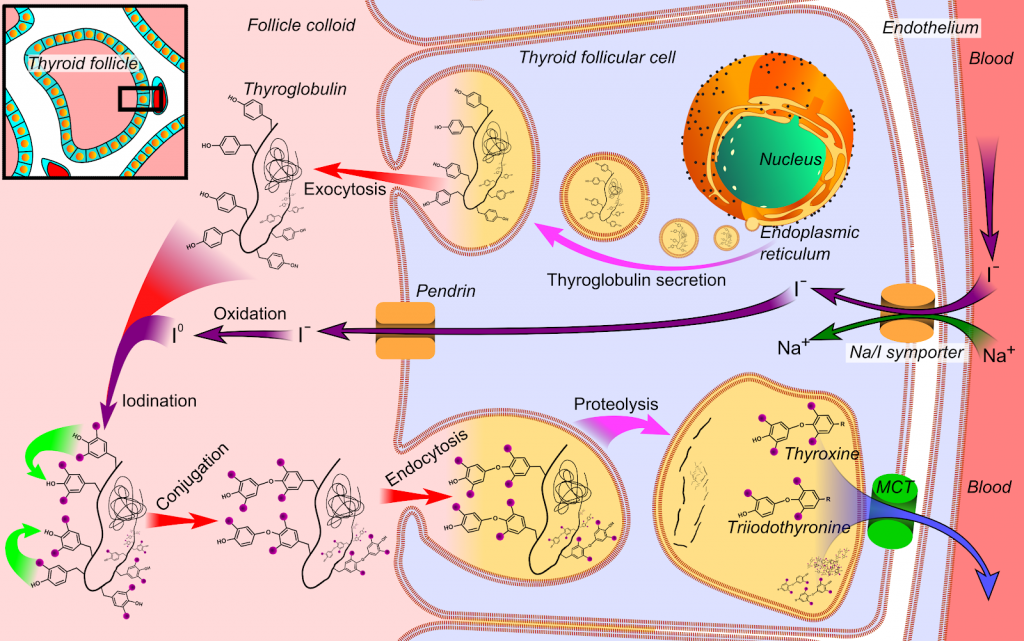
Iodide is oxidized into iodine, and then we have iodination along thyroglobulin. What happens, though, and what we are seeing here is that iodine has formed these things that can be found along thyroglobulin.
It used to be thought that a molecule of thyroglobulin would contain four iodine atoms, thus making it T4. We have a little bit more knowledge these days, though, and we now know that a molecule of thyroglobulin can make many different molecules of T4 and T3.
And, it is common to have one contain about 10-11 iodine atoms altogether. However, in cases of high iodine, this same molecule could have as many as 60 iodine atoms.
Think about it like a coat rack. You have 8-10 hangers available, but you could also throw coats on top of coats on top of coats, and in that case you might not even be able to get to the hooks you had there in the first place!
That’s what happens here. The whole molecule gets completely blanketed by iodine. When that occurs, all this extra iodine damages that molecule as well as the enzyme that helps the process happen in the first place.
That is thyroperoxidase. Thyroperoxidase becomes oxidized, and your immune system begins to attack it. The thyroglobulin also begins to look foreign, too, so the extra iodine recruits immune cells and targets them against thyroglobulin.
Key Insight: This is what we know now to be the genesis of so much of autoimmune thyroid disease. Your immune system attacks thyroglobulin, and thyroperoxidase, all while damaging the surrounding cells in the area.
How Iodine Initiates Autoimmune Thyroid Disease
These free radicals from the unpaired iodine, have been shown to injure the cells in both human and animal models.5
Studies have also shown that, if you give animals a mega-dose of iodine, but you pre-treat them with a drug that prevents iodine from forming free radicals, it doesn’t trigger thyroid disease in the same way.
That is all to say that we know iodine in excess can be a culprit, because what it’s doing is heightening the production of cytokines and chemokines. These cause the cells to go after the thyroid.
In the next stage, these cells have more and more damage and become unable to make hormones. Finally, in the last step, the immune system has been alerted to this damage and become sensitized against those very thyroid cells.6
How Does Iodine Cause Postpartum Thyroiditis?
This is a version of acute thyroiditis. It comes on quickly, and after delivery, and is more common in women that have high thyroperoxidase antibodies, and it is more common in those that have had more iodine exposure.
In human studies, we have seen that the median amount of iodine in women with postpartum thyroiditis is about 40% higher than those who do not develop it. This is proof that iodine can be a causative factor in this process.7
How Does Iodine Cause Thyroid Cancer?
Iodine plays a relevant role here. While there aren’t clear singular mechanisms, it is thought that iodine can act as an initiator of thyroid cancer, but more as a weak promoter of thyroid cancer.8
We can see some evidence from clinical studies. One study, in particular, included more than 4,000 patients with thyroid papillary cancer. What they found was that 43% of those people had unusually high amounts of iodine.9
Another study of those with thyroid cancer found that 47% of them had elevated levels of iodine. This is much higher than we would normally see in populations without thyroid cancer.10
How Does Iodine Make The Thyroid Overactive?

Is there a way in which iodine relates to hyperthyroidism? The evidence would suggest that there most definitely is a connection.
This has been called “iodine-induced hyperthyroidism,” also called the Jod-Basedow effect. Basically, what happens is that massive amounts of iodine can cause the immune cells to target outside of the thyroid.
In those cases, the thyroid acts as if TSH is present, because the immune cells mimic the effect of TSH. One study, with over 400,000 people, saw that early hyperthyroidism went up by 64% with even the tiniest increase in iodine disease.11
Key Insight: We also see that those that have higher rates of iodine exposure have lower rates of going into remission from things like Graves’ disease.
One study showed that even when iodine went up in small amounts, the remission from Graves’ went from 60-80% of people feeling better almost at random, to 13-20%.12 That is a shocking change in the number of people getting better due to higher iodine levels.
What About Toxic Nodular Goiter?
This is a condition that is classically set off by a radical increase in the dietary intake of iodine. That can be from in the diet or from iodine in medications/in contrast agents13.
How Does Iodine Cause Goiter?
This is one where it goes both ways. That’s because severe deficiencies can cause goiter, as can severe iodine excess.
As of 2014, the severe levels of deficiency are longer present on planet Earth (that is per the World Health Organization). At the same time, though, we now have 52 countries that are in varying regions of excess.14
One study revealed that areas that had high amounts of iodine in the water, these areas had a rate of goiter that was present in 65% of individuals.15
In the same area that didn’t have it, goiter was virtually nonexistent. So, in this way, it is so important to remember that high iodine, too, can cause goiter.
How Does Iodine Cause Hypothyroidism?
When it comes to congenital hypothyroidism, this is one of the worst things out there. We have strong evidence that babies can be born with low thyroid function because of their mother’s exposure to too much iodine.
This is what we call “Wolff-Chaikoff in utero.” This is tragic because it is completely unnecessary and avoidable, typically caused by iodine supplements that didn’t need to be taken in the first place. It’s really sad stuff.16
The True Effects of Iodine
As we have discussed together, the true effects of iodine are incredibly varied and can run the gamut from congenital hypothyroidism to thyroid cancer.
That is why it is so important to know more about it. The number of iodine matters, because it is, to date, the single-biggest driver of thyroid disease.
But, the complicating factor is that we do need some! That said, we can’t have too much, too little, or even an erratic amount. It needs to be the exact right amount.
As things stand, there is far more risk of getting too much iodine these days than not enough. That is why you need to be conscious of sources and where you might be getting it.
Discover Your Ideal Range Today
The good news of today’s story is that, when you are within the ideal range, you have the opportunity to not only stop the disease but for many, it can get better.
That’s why I want to share this information with you. Not to scare you or to have you swear off iodine, but to help you feel your best and to do it with the science at your back.
Do you want to start recovering? Take the Thyroid Quiz today (click here for the quiz) to discover where you stand and how we can work together to help you feel better.
Resources
2 – https://pubmed.ncbi.nlm.nih.gov/11396709/
3 – https://pubmed.ncbi.nlm.nih.gov/9703374/
4 – Häggström, Mikael (2014). “Medical gallery of Mikael Häggström 2014”. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.008. ISSN 2002-4436.
5 – https://www.ncbi.nlm.nih.gov/pubmed/10222025/
6 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4139880/
7 – https://pubmed.ncbi.nlm.nih.gov/16419489/
8 – https://www.ncbi.nlm.nih.gov/pubmed/26146517/
9 – https://pubmed.ncbi.nlm.nih.gov/30910201/?from_term=iodine+thryoid+cancer&from_exact_term=iodine+thyroid+cancer&from_pos=7
10 – https://pubmed.ncbi.nlm.nih.gov/28258306/
11 – https://www.ncbi.nlm.nih.gov/pubmed/9553166/
12 – https://www.ncbi.nlm.nih.gov/pubmed/2443050/
13 – https://medlineplus.gov/ency/article/000317.htm
14 – https://www.who.int/vmnis/database/iodine/iodine_data_status_summary/en/
15 – https://pubmed.ncbi.nlm.nih.gov/2886725/
16 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4354797/#:~:text=Excess%20iodine%20ingestion%20from%20nutritional,milk%2C%20can%20cause%20neonatal%20hypothyroidism.&text=Three%20cases%20of%20infants%20with,by%20newborn%20screening%20are%20presented.
1. Schedule a Thyroid Second Opinion with me, Dr. C, Click Here for Details
2. Download and use my Favorite Recipes Cookbook Here
3. Check out my podcast Medical Myths, Legends, and Fairytales Here
Dr. Alan Glen Christianson (Dr. C) is a Naturopathic Endocrinologist and the author of The NY Times bestselling Adrenal Reset Diet, The Metabolism Reset Diet and The Thyroid Reset Diet.
Dr. C’s gift for figuring out what really works has helped hundreds of thousands of people reverse thyroid disease, lose weight, diabetes, and regain energy. Learn more about the surprising story that started his quest.


