Hyperparathyroidism: The Truth

I had never heard about hyperparathyroidism until I reached medical school. The impression that it got was that it was:
- Rare
- Caused unusual/recognizable symptoms
- Easy to diagnose
Key Insight: If you have symptoms that include some mixture of fatigue, digestive issues, anxiety, or muscle aches, this could be the hidden reason. If you have thyroid disease, your risks for parathyroid disease are higher.
Over the years of treating thyroid disease, I have come to realize that none of these things are true. It is not rare and it can cause the most common symptoms we suffer from. In fact, it is easily missed unless a doctor knows exactly how to find it.
I would love to be able to give you a really good understanding of parathyroid disease, and what you need to know about it. So that you can know for sure if this applies to you. In addition, which next steps you can begin to take.
Jonell’s Story
“Jonell” was a patient of mine in my early years of practice. Like most, she first came in already on thyroid treatment but was not at her best just yet.
A bunch of symptoms came on around the same time and she thought her thyroid was the culprit.
Once diagnosed with thyroid disease, she went on treatment and it did get easier to manage her weight. However, her symptoms of IBS, fatigue, and anxiety did not get any better.
She hoped that if I helped her optimize her thyroid treatment that they could improve also.
For the first steps, we helped her liver function, improved her micronutrient levels, and dialed in her medication.
She did improve with these steps, but not as much as she or I would have liked. It seemed like certain foods triggered reactions but it also seemed like the more foods she tried, the more foods she reacted to.
Considering Less Common Culprits
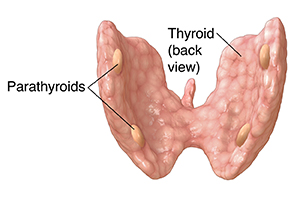
“Para” means next to and the parathyroid glands are located next to your thyroid. Typically people have four parathyroid glands, two on each side of the lower portion of their thyroid.
However, there is some variation in:
- Their location
- How large they are
- How many there are
The parathyroid glands secrete parathyroid hormone (PTH), also called parathormone or parathyrin. It pulls calcium out of your bones and into your bloodstream.
It works in opposition with a thyroid hormone called calcitonin which mostly moves calcium out of the blood and into the bones. One of the reasons that overdosing on thyroid hormones hurts the bones. It blocks the gland from releasing calcitonin.
Back to Jonell’s Case…
After seeing this elevated level of calcium, I decided to test her parathyroid function. I was not highly suspicious of it being abnormal because her blood calcium was normal all the rest of the time. Instead, I was trying hard to find something.
Her retest showed that her calcium levels were fine but parathyroid hormones were 50% higher than normal. These findings were diagnostic of primary hyperparathyroidism.
I referred Jonelle to a local surgeon who specializes in parathyroid disease. He evaluated her and agreed with the diagnosis. Within weeks after surgery, her symptoms were better than they had been in years.
She found that she could eat a broader range of foods. Jonell also noticed that normal life stressors did not trigger her anxiety the way they did in the past. We also found it easy in the following months to keep her thyroid levels regulated with less testing and adjustment.
Bottom Line: Jonell’s case radically changed the way I’ve come to understand parathyroid disease. Many doctors have been taught that unless there are high levels of blood calcium, parathyroid disease is not possible. This is not true.
Key Insight: High levels of blood calcium are never insignificant and always need to be diagnosed. Besides parathyroid disease, the next common culprits are hidden cancers or kidney disease. None of these should ever be missed.
- Primary
- Secondary
- Parathyroid cancer
Primary Hyperparathyroidism

In the case of primary hyperparathyroidism, the parathyroid glands have grown some unhealthy cells (adenoma) and are making too much parathyroid hormone (PTH).
80% of the time, with PHPT, a single parathyroid gland is overactive. In 15-20% of cases, multiple glands are involved.1 If this goes on to a large enough degree in a long enough duration, it can cause higher levels of calcium in the blood.
- Some cancers
- Vitamin D overdose
- High levels of thyroid hormones
- Abnormal adrenal function (Read: The top 3 myths of adrenal fatigue)
Key Insight: If vitamin D levels are low, they can trigger parathyroid disease. However, too much is also not good. If vitamin D levels are too high, they can unmask latent parathyroid disease.2
Secondary Hyperparathyroidism
Secondary hyperparathyroidism is completely different. In a case like this, the parathyroid glands are working harder for a good reason because the body is losing too much calcium.
The most common reason for this is kidney failure, and can also occur due to severe deficiencies of calcium or vitamin D.

Parathyroid Cancer
The rarest of all types of hyperparathyroidism is parathyroid cancer.
This represents 1% or less of the cases and it occurs when the parathyroid glands develop a malignant overgrowth of cells.
Hypoparathyroidism
The parathyroid glands can also become underactive. This is called hypoparathyroidism. When it does happen, it is most common after surgery to the thyroid or the parathyroid glands.
In rare cases, this can occur soon after birth or later in life for no clear reason. For the remainder of our discussion, we will be talking about primary hyperparathyroidism (PHPT) which I will refer to as parathyroid disease.
How Common is Parathyroid Disease?
Like thyroid disease, parathyroid disease is more common in women. The ratio is about 3:4 (women to men).
In 2008, it was estimated that 0.86% of the US population was diagnosed with hyperparathyroidism.
Key Insight: For comparison’s sake, this is roughly as common as celiac disease. The rates have tripled in some areas like California, most likely due to better screening.
However, in those with thyroid disease, hyperparathyroidism may be six times more common.3
What Causes Parathyroid Disease?
By in large, parathyroid disease comes on unexpectedly and for no clear reason. There are known genetic components, and no known risk factor for those who have a family history.
In addition, early-life radiation to the neck is known to be a large risk factor. In the past, it was common to have tonsils irradiated as a treatment for tonsillitis and this was a risk factor.
Exposure to certain medications can also be a risk factor. Those with the most documentation include lithium and thiazide diuretics such as hydrochlorothiazide.4
Hyperparathyroidism can also show up by itself or, more rarely, in a cluster endocrine-related cancer called multiple endocrine neoplasia syndrome (MENS).
This condition is more common for those who have a family history of the condition.
Overlap With Thyroid Disease
People who have thyroid nodules have a higher risk of PHPT. Those who have had to have thyroid surgery also have higher risks for it.5
In the case of Hashimoto’s thyroiditis, the risks for parathyroid disease may be 6 fold higher than it is in the general population.
Some estimates say that there may be as high as a 5% overlap between autoimmune thyroid disease that may have parathyroid disease.6
Other Disease Risks
Ultimately, untreated parathyroid disease raises the risk, long term, of:
- Heart attack
- Stroke
- Congestive heart failure7
It has also been shown that the higher one’s serum calcium is for an extended period, the greater the risks are for breast cancer.
There is also known overlap between parathyroid disease and esophageal and oral cancers.8
What Are Symptoms of Parathyroid Disease?
In medical school, we were taught a mnemonic to memorize the symptoms associated with parathyroid disease: “Stones, bones, moans, groans, thrones, and psychic overtones.”
These categories can be useful ways to think about how abnormal parathyroid levels in calcium levels can affect the body in which symptoms arise from that…
Stones
Because calcium levels are too high, people are at greater risk for kidney stones. There is also some evidence that gallstones and gallbladder disease are more prevalent with parathyroid disease.9
Bones
When parathyroid glands release too much hormone because a higher rate of release of calcium from stores in the bones.
Overtime, this can lead to:
- Arthritis
- Bone pain
- Early thinning
- Osteoporosis
- Hip and spinal fractures
Moans
Optimal levels of blood calcium are essential for nerve conduction and almost every part of normal biochemistry.
The classic symptoms include:
- General malaise
- Fatigue
- Lethargy
- Muscle pain
Groans
The term ‘Groans’ refers to gastrointestinal symptoms. When calcium levels are abnormal, the digestive fluids are not secreted properly.
This can trigger all of the classic symptoms that get misdiagnosed as IBS, SIBO, or heartburn:
- Constipation
- IBS
- Bloating
- Nausea
- Vomiting
- Ulcers
- Hyperacidity
Thrones
This one is probably the least intuitive, but it did make for a handy rhyme.
Ever heard of the “porcelain throne”? People with parathyroid disease can have severe constipation that does not respond well to typical treatments.
They may also have an abnormally high thirst and, therefore, frequent have troublesome urination.
Some even end up having to spend a lot of time on the throne.
Psychic Overtones
The brain is far from immune to the effects of normal calcium levels. It renders it far less able to carry out its proper cellular interactions.
I have seen many patients with debilitating anxiety that led to years of unsuccessful treatments through medication, talk therapy, or lifestyle. Only to disappear in a matter of days after treatment.
Common symptoms here can include:
- Anxiety
- Confusion
- Depression
- Memory loss
- Brain fog
- Difficulty walking
You can see that these symptoms are numerous and common.
Some, like anxiety, fatigue, and muscle pains, are symptoms that doctors all too often give up on finding explanations to help diagnose and treat.
Do you have parathyroid disease?
In classic cases, hyperparathyroidism shows up with elevated levels of calcium in the blood.
Too often, though, patients are told that elevated calcium is not significant.
It always is and should never be ignored. But, the even tougher part is that many doctors do not know that it can also show up with normal levels of blood calcium.
Key Insight: Because PTH is not routinely used as a screening test, a doctor can completely miss hyperparathyroidism in someone with normal calcium levels unless they are suspicious enough to dig deeper.
- Elevated and the parathyroid gland is working correctly, it will lower its production of PTH. PTH will be low and the calcium is high for some other reason.
- High and the PTH is normal or elevated, the parathyroid glands are not working correctly.
Here is where it gets tricky. For 20% of people with hyperparathyroidism, their calcium levels are not elevated.
If someone has high-normal levels of calcium and they have good parathyroid function, their PTH should be low.
If not, they have primary hyperparathyroidism.
Breaking Down the Data
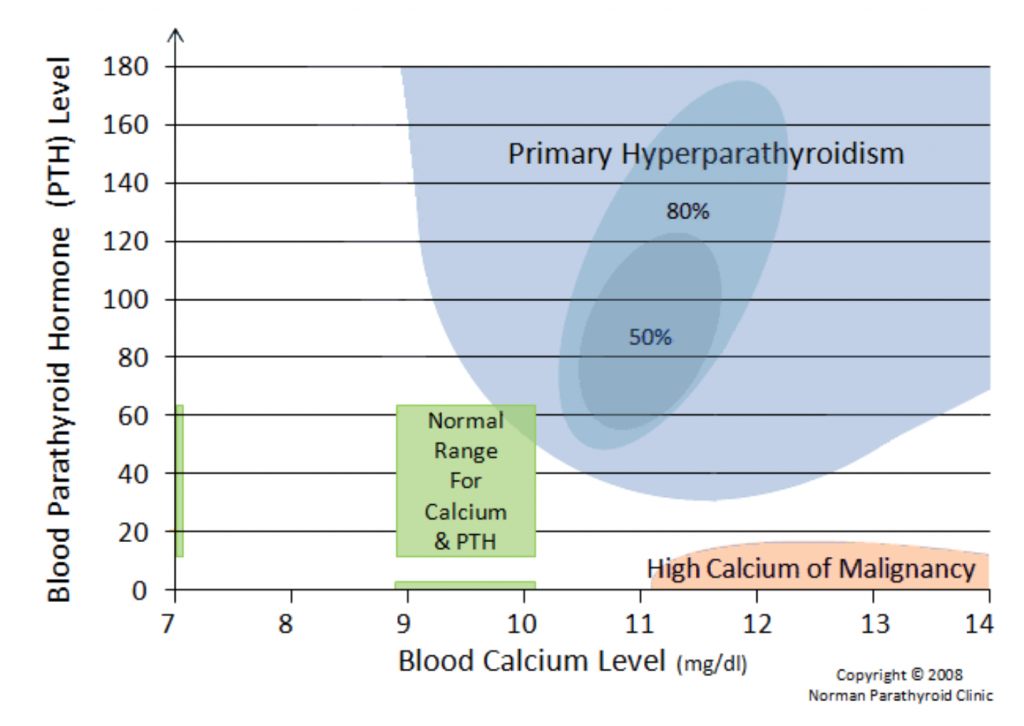
Here are some images courtesy of parathyroid.com, which is a production of the Norman Parathyroid Center. Both are excellent resources for parathyroid information and care.
In the first image, you can see that ‘normal’ blood calcium levels in the range of 9.8 – 10.5 can still be associated with hyperparathyroidism and symptoms of hypercalcemia.
You can see that a large number of patients with hyperparathyroidism have normal calcium levels (some even have normal levels of both calcium and PTH).
How would you know they had hyperparathyroidism if both calcium and PTH were normal? If one is up, the other should be down.
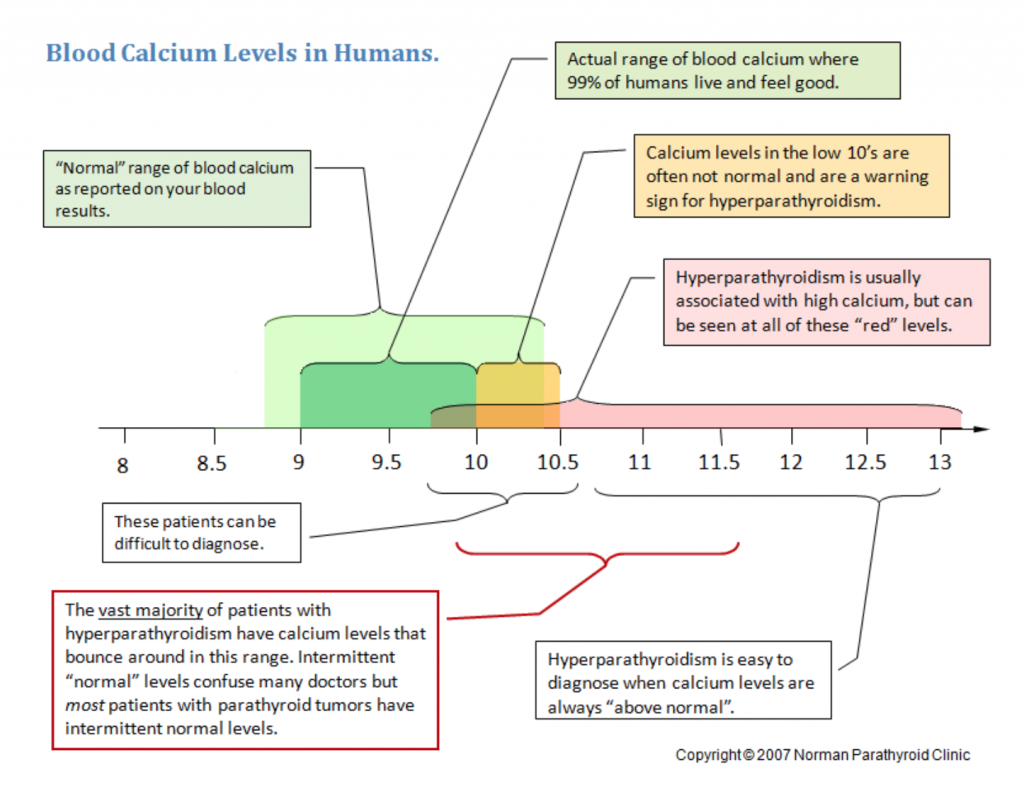
In the case they both are on the higher side of normal and the person has suspicious symptoms, there may be a problem.
What Doctors May Assume
Many doctors assume that high calcium and high PTH must be present and that kidney stones and distinct patterns of bone loss must be present.
There definitely are patients in which all of these findings are present. However, in over 80% of those with parathyroid disease, they are not.
There are other ways of evaluating calcium by calculating albumin-corrected calcium or measuring ionized calcium.
These methods can make hypercalcemia more evident when patients serum calcium is high normal but they are not necessary for diagnosis and do not prevent the need for measuring PTH levels.
The following table can summarize the diagnosis based on serum calcium and PTH:
| Calcium (8.5 – 10.4 mg/dL) | |||||
| Low | Normal | High normal | Elevated | ||
| PTH (10-65 nmol/L) | Low | hypoparathyroidism | hypoparathyroidism | High calcium – excessive intake, malignancy | High calcium – excessive intake, malignancy |
| Normal | hypoparathyroidism | Healthy | Primary hyperparathyroidism | Primary hyperparathyroidism | |
| Elevated | Secondary hyperparathyroidism
Low calcium: low intake, chronic kidney disease, etc |
Primary hyperparathyroidism | Primary hyperparathyroidism | Primary hyperparathyroidism | |
How is parathyroid disease treated?
The answer is quite clear: Surgery.
There is no diet, supplement, essential oil, or medication that will help primary hyperparathyroidism. Roughly, around 95% of the time, surgery is curative.
When surgery does not work, it is almost always because the surgeon failed to find all the overactive parathyroid glands. In these cases, follow-up surgery is nearly always curative.
Complications are rare but include damage to the recurrent laryngeal nerve. This can impact speech and swallowing.
The remaining parathyroid glands can be damaged. This can leave them underactive or spur them into overactivity.
In the rarest complications, the thyroid gland can be traumatized by surgery and change how it works.
Bottom Line: The success of the surgery and the rate of complications is highly dependent on the experience of the surgeon. The glands can be hard to see during surgery. It also may not be clear which of the glands are involved. It is worth working with one of the small number of surgeons who specialize specifically in parathyroid surgery.
What Does the Process Look Like?
In the hands of the right doctor, the whole procedure can take as little as 20 minutes and may not even require general anesthesia.
I can think of very few situations that affect health so deeply that can be resolved that quickly.
There is a medication called cinacalcet (Sensipar) that “looks” to your parathyroid like PTH and may lower its activity. They are appropriate for hyperparathyroidism secondary to dialysis.
Some doctors may offer this in place of surgery but new data shows it is harmful and that surgery is still the best answer.10
What happens after surgery?
Nothing, really.
Good surgeons are able to leave healthy parathyroid glands intact. It is helpful to get enough calcium after surgery so that they do not have to work too hard.
Once the first few weeks have passed, the remaining glands pick up the slack for those that were lost and the calcium balance is normal again.
What should you make of this?
Serum calcium is a typical part of nearly every routine blood tests.
If your levels have ever been elevated, please work with a good doctor to find out why that is the case.
Have you had any ongoing symptoms like:
- IBS (Read: IBS the top 4 warning signs people miss)
- Bloating
- Mood changes
- Anxiety
- Fatigue
- Constipation
- Frequent urination
- Muscle pain
- Brain fog
Key Insight: If you have been unable to improve the symptoms, even if you and your doctor think you know why they are happening, please do consider hyperparathyroidism.
Next, your best step forward is to have a doctor who is familiar with this condition do proper testing and see if it may be relevant for you.
Not only is it important to treat because it may resolve troublesome symptoms. If it is not identified, it can create other problems that can shorten your lifespan.
Resources
2 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4663778/
3 – https://www.ncbi.nlm.nih.gov/pubmed/23865082
4 – https://twin.sci-hub.tw/6635/1c2f138b1a2fdf710095845684ff6649/bilezikian2017.pdf?download=true
5 – https://www.ncbi.nlm.nih.gov/pubmed/19040989
6 – https://www.ncbi.nlm.nih.gov/pubmed/23865082
7 – https://academic.oup.com/eurheartj/article/25/20/1776/497057
8 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3603029/
9 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6014369/
10 – https://www.parathyroid.com/Sensipar-high-calcium.htm
1. Schedule a Thyroid Second Opinion with me, Dr. C, Click Here for Details
2. Download and use my Favorite Recipes Cookbook Here
3. Check out my podcast Medical Myths, Legends, and Fairytales Here
Dr. Alan Glen Christianson (Dr. C) is a Naturopathic Endocrinologist and the author of The NY Times bestselling Adrenal Reset Diet, The Metabolism Reset Diet and The Thyroid Reset Diet.
Dr. C’s gift for figuring out what really works has helped hundreds of thousands of people reverse thyroid disease, lose weight, diabetes, and regain energy. Learn more about the surprising story that started his quest.


