The Role of Iodine in Medicine
Iodine is neither a good thing nor a bad thing. It is an essential nutrient we need in exacting amounts. So, how much iodine is safe per day? There’s a specific number you need to know. Apart from its role as a nutrient, it is a really useful chemical. It is one of several elements in a group called halides. Other halides include chlorine (bleach), fluoride, and bromide. Like other halides, Iodine is a strong free radical generator, and that gives it a lot of helpful properties.In the early years of medicine, these properties made iodine compounds useful as an:
- Antiseptic
- Expectorant
- Anesthetic
- Antiparasitic
- Contrast agent
Starting around the 1950s and ’60s, doctors got better at tracking things. They started noticing thyroid complications from iodine treatments. Iodine started to go by the wayside as doctors found safer alternatives.
A recent example was in the case of hand sanitizers. In 2017 the FDA restricted the usage of iodine1 in them when it was found that health care workers who used them were often found to have unsafe levels of iodine.
How much iodine is safe per day?
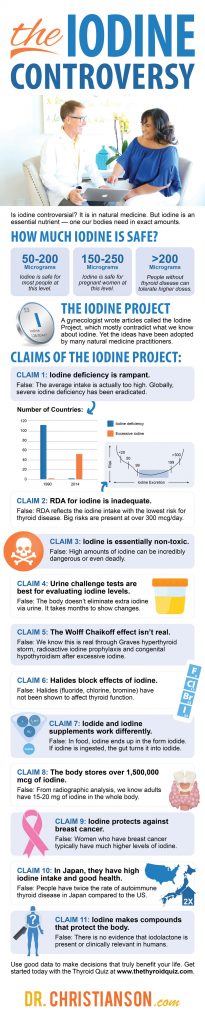
Let’s cover this important point before we go any further: How much iodine is safe per day? The World Health Organization (WHO) has stated that, for those who do not have thyroid disease, may safely be exposed to iodine as high as 1100 mcg/day. Data shows that things are different for those who have or are prone to thyroid disease. For them, the safe upper limit appears to be closer to 200 mcg. Please keep these numbers in mind as we talk through the Iodine Project.The Iodine Project
In the late 1990s and early 2000s, a gynecologist wrote a series of articles he called the ‘Iodine Project’. They were the sole source of ideas like high dose iodine helps thyroid disease, or urine or blood tests are good tools to check iodine levels, or chemicals like bromine blocking the effect of iodine. These ideas alone contradicted the last century’s worth of research on iodine. That said, they have been taken up — uncritically — by some practitioners of natural medicine.Why Have These Ideas Spread?
Even if they don’t fit the data, these ideas have spread and have become popular in certain circles. I think this is based on three different reasons that they are:- Familiar – We are simply missing a vital nutrient
- Plausible – In that iodine is essential for thyroid function
- Palatable – It presents as a simple and low-cost solution
My Personal Experience With These Ideas
Somewhere around 2005 or 2007, the ideas of the Iodine Project became pervasive. By this point, I was seeing new patients almost weekly who developed thyroid disease after attempting high dose iodine. This gave me a great range of exposure to many different treatment types — and the very real effects that they had on people I was trying to help.Key Insight: Both conventional and non-conventional, I have seen how many ideas and treatment types have played out for people in real-time.
Patient #1: Richard
One of the first experiences I had with this was with a patient who I will call Richard (not his real name, of course). Richard was a gentleman who was in Michigan half the year, and Arizona the other, and was inspirational in his commitment to both his health and fitness. In his mid-70’s, he was a flawless physical specimen. One year he came down, and he had a rare type of thyroid disease that he came to see me about. This came about after he received the results of a test telling him that he had an iodine deficiency. After he started treatment, he developed this version of thyroid disease. It turned out that he had this iodine challenge test done, and that seemed to correlate with the onset of his thyroid disease. The doctor told him that, due to his iodine deficiency, he needed the iodine, that they were lucky to have caught it, and that if he took enough of it, the toxic nodular goiter that he had may go away. But, I knew that this type of issue was likely to come about after high exposure to iodine. Around this same time, there were many people who were undergoing the same thing. They were receiving massive amounts of iodine, and it was revealing thyroid disease.Patient #2: Jenny
Another was a woman I will call Jenny (again, not her real name). Her doctor ran an iodine test on her and told her she also had an iodine deficiency. He said that if she took iodine she could lose weight more easily. Within a few weeks, she developed troubling symptoms like:- Palpitations
- Hair loss
- Mood shifts
My Own Writing
At this same time, I was also writing the Complete Idiot’s Guide to Thyroid Disease. What I wanted to do was talk about iodine, and to get it right. I knew it was so crucial to know more about it, so I wanted to ensure I was providing absolutely all of the facts. This inspired conversations with the doctor who started the high iodine movement. The main reason that I wanted to see his work was that I wanted to dive a bit deeper into his references. I had already heard his main claims, but I wanted to see the proof. I decided to reach out to him personally. Despite the fact that I came to disagree with him, it should be known that he was kind and sincere. He made himself available to me and was gracious with his time. After our first conversation, he mailed me a massive box with hard copies of all the things he had written, some of which he had not yet published. I felt myself being torn as I got deeper into his work. He struck me as a good man who wanted to help people. I can respect that. Yet it became undeniable that the information he was writing was not accurate. And more and more of my patients were suffering needlessly because of following this approach. After reading all of his writings, his references typically fell into one of three major categories:- Old – Many citations were from the 1920s to the 1940s. These were largely based on speculations made when we knew much less than we do now.
- Animal-based – Many other references were to findings that were not derived from humans.
- Circular – The majority of his references were to his own work. I often followed a never-ending trail of references that went around in a circle.
What We Know About ‘Iodine Deficiency
Over the next few months, I read everything I could about what science did know about iodine and thyroid disease. The current evidence showed that medicine moved away from the use of iodine because its harms became more apparent with better research. Over the years evidence kept showing that iodine could be harmful at doses lower than previously suspected. The safe range kept getting narrower and narrower.Key Insight: The new model is that iodine has the narrowest safe range of any known nutrients. In that sense, it can be known as the “goldilocks mineral.”
Iodine has been shown to trigger thyroid disease with:
- Too much
- Too little
- Too variable
The most uncanny thing about iodine is that the ideal window is narrow. The best daily intake only has a range of about 50 mcg before you start to get too much or too little!
The Main Claims of the Iodine Project
1. Claim: Iodine Deficiency Is Rampant
Specifically, the Iodine Project has stated that the US iodine supply has gone down 50% or so in the last 30 years.
The story does get more complicated. Levels did go from excessive (320 ng/ml) in 1970 to adequate (170 ng/ml) by the early 1980s.
Yet from 1988 to 2008, the average intake has gone up and the variation in iodine intake has gone up tremendously. Some people are now getting much more than others. Prior to the 1980s, most people were getting about the same amounts.
The chart below shows how iodine intake increased in most groups from the 1980s to the 2010s.2
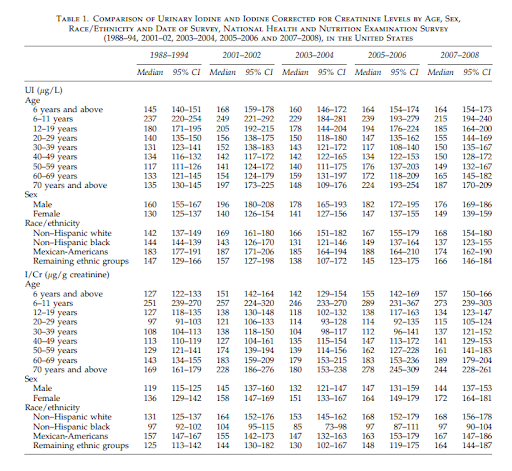
| Percent of the US population at unsafe iodine level (≥ 200 µg/L) | ||||||
| Gender | Ethnicity | Age | ||||
| 20-29 | 30-39 | 40-49 | 50-59 | 60-69 | ||
| Female | NWH | 36% | 35% | 31% | 33% | 34% |
| NHB | 19% | 23% | 33% | 37% | 33% | |
| MA | 33% | 41% | 32% | 40% | 35% | |
| Male | NWH | 37% | 35% | 46% | 41% | 48% |
| NHB | 29% | 27% | 33% | 32% | 44% | |
| MA | 35% | 47% | 45% | 40% | 47% | |
Who Is Low In Iodine?
When the Iodine Project claimed people are getting too little iodine, they pointed to studies on iodine in pregnancy (Click Here: How Much Iodine Do You Need?). There have been studies showing that pregnant women have been lower in iodine yet we are not seeing complications in mothers or babies from a low iodine intake. How can this be? In more recent years we have learned that pregnant women do best on a lower amount of iodine than was thought in the past. We also know that they are at risk for too much at a lower threshold than previously thought. It’s important to consider how iodine works during pregnancy: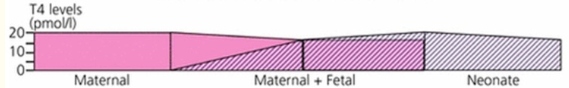
This chart illustrates why a mother’s levels can fluctuate quite easily. The needs are different because of a distinct transition that occurs.
In the first trimester, the baby’s thyroid hormone comes from the mother, and as the fetus develops it slowly develops its own thyroid hormone, so it no longer needs it from the mother.
This is especially true for those in the late-second and third trimester because fetuses start making all of their own thyroid hormones by that point.5
The largest study to date on iodine intake and thyroid function among pregnant women was just completed. It showed that women consuming just slightly excessive amounts of iodine had high rates of hypothyroidism, maternal hypothyroxinemia, and thyroid autoimmunity.6
Again, it is a matter of getting it right. Too little iodine during pregnancy could cause cognitive delays.
Thankfully that is no longer a common event. The most recent examples were Papua New Guinea in the 1960s and a remote province of China in 1990.
Both of these areas at the time had endemic cretinism.7 This is a congenital disease from iodine disease, stemming from iodine deficiency.
It seems that with iodine in pregnancy, mild deficiencies are less harmful on the baby and the mother than mild excesses. In the modern world, pregnant women with what was considered a mild to moderate iodine deficiency no longer have infants with developmental delays.8
How Much Iodine Is Best For Pregnant Women?
Complications emerge when mothers are under 50 mcg/L. Our latest guidelines suggest that the ideal range is a level of 150 – 250 mcg/L.
Let’s take the following passage for example:
“The risks of even mild iodine excess in pregnancy need to be carefully considered. The lowest prevalences of hypothyroidism, hypothyroxinemia, and thyroid autoimmunity, as well as the lowest serum thyroglobulin levels observed in the women with UIC of 150–249 µg/l”9,10
Do Pregnant Women Need Iodine Supplements?
The fact is that around 75% of OB and midwives do not recommend iodine supplements for preconception, pregnancy, or lactation.11
In addition, the ACOG and the AACE do not recommend it, either. That is, in the case of the AACE, unless it is mandated specifically to a geographic region.12
Finally, the American Thyroid Association states that:
“Without specific physiologic evidence of iodine deficiency in the United States at this time, and with the most recent U.S. survey reporting a median value of 173 g/L, which is within that currently recommended for pregnancy, the rationale for iodine supplementation during pregnancy is tenuous”13
A review, known as the Cochrane review, pulled together all of the current data over the last decade and culminated what we know about iodine during pregnancy.
They found that supplementing iodine during pregnancy:
- May worse nausea and vomiting
- May elevated maternal thyroid antibodies
- Has no clear effect on maternal thyroid disease
- Did not affect the rate of preterm births
- Did not affect the baby’s risk of thyroid disease14
- Studies on preterm infants have also shown no benefit to iodine supplementation15
Iodine Deficiency Globally
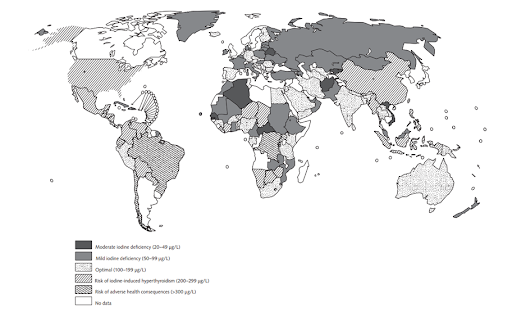
If the US is not iodine deficient, what about the rest of the world?
Globally, the idea of iodine deficiency has completely changed in the last few decades.16 Many nations used to be severely deficient, now none are.
Let’s take a look at this quick comparison chart.
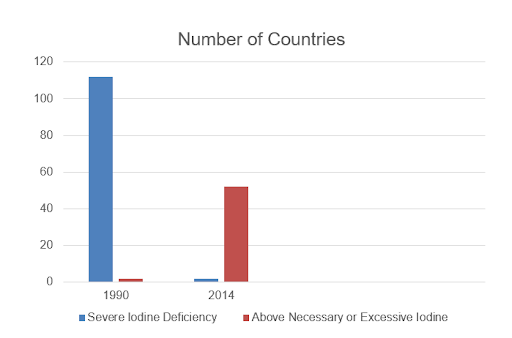
Bottom Line: The US is not iodine deficient. Globally, severe iodine deficiency has been eradicated.
2. Claim: The RDA of Iodine Is Inadequate
Another popular claim of the Iodine Project is that adults need much more than the recommended daily allowance of 150 micrograms. Those in the project argued that we need 14,000 – 15,000 micrograms. The sweet spot for us appears to be between 50 – 250 mcg per day, and this is based on numerous population studies which can be summed up in this chart: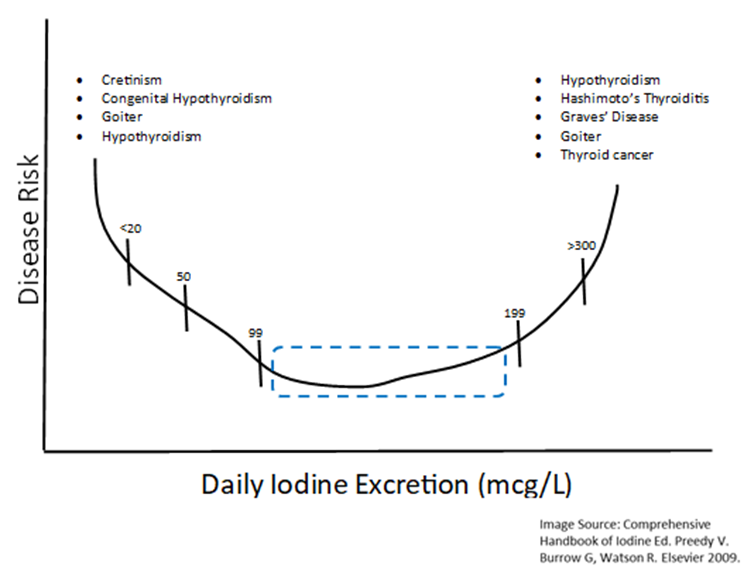
This is a compendium of hundreds of human studies, of different populations, showing the risk for thyroid disease based on the amount of iodine exposure.
What we see is what we call a C or J-shaped curve. This is to where, with severe iodine deficiency, there is a greater risk for thyroid disease.
At the same time, the same is true of iodine excess. There is risk that exists there, too, for thyroid disease. That window translates to our window of around 50 – 250 mcg.
The WHO has been doing this research, as well.17 They have even illustrated how different levels of iodine intake correlate with different types of disease, here it is:
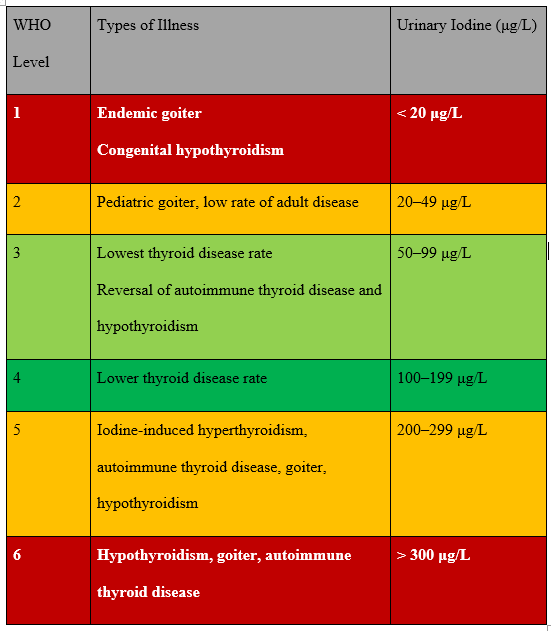
As you can see from the above, over 300 mcg per day and you can have serious health risks present. That is why it is so dangerous to recommend an even higher intake of iodine.
Key Insight: The RDA for iodine reflects the iodine intake that gives the lowest risk for thyroid disease.
3. Claim: Iodine Is Essentially Non-Toxic
Here is a quote from the Iodine Project that will start us off:
“The toxicity of iodine depends on the forms of this element. . . The man made organic forms of iodine are extremely toxic, whereas the inorganic non-radioactive forms are extremely safe”18
What they refer to as the “man made organic forms” are basically iodine in drugs, or radioactive iodine used in ablation (or other forms of synthesized iodine) (Click Here: Your Guide To Radioactive Iodine).
On the other side of things, what they are calling natural forms of iodine include:
- Potassium iodide
- Iodine in Lugol’s solution
- In various foods
- In supplemental form
What they are arguing is that iodine, in these above forms, is extremely safe.
So, we basically have a registry of all known chemicals and all their toxic profiles. From that registry, they have a lot of entries on iodine.
There is a range of iodine intake where its harmful effects are limited to the thyroid. But above some threshold, iodine can be toxic to the entire body.
The main tissues affected include the:
- Skin
- Heart
- Lungs
- Kidneys
- Intestinal Tract
- Liver
- Blood
- Neuromuscular system
- Brain
- Skeleton
- Pituitary and adrenal glands
A tragic example of iodine’s toxicity In fact that ingesting it was once the most common means of suicide.
Have you ever seen a historic iodine bottle with the skull and crossbones? They were there for a reason.
There is an iodine supplement, Iodoral, and it comes in two potencies:
- 12.5 mg
- 50 mg
If you go onto medical databases and put in Iodoral, you will not find many case reports about people who have been harmed by it. In fact, one case report I came across noted:
“Severe, symptomatic hypothyroidism induced in 2 patients with underlying autoimmune thyroiditis (Hashimoto’s disease) following ingestion of Iodoral™”19
This next part is especially troubling. Assuming organic iodine to be harmless, a recent book by another doctor advises pregnant women to follow the same advice he recommends for adults — to use 12.5 – 25 mg of iodine daily.20
I will come back and talk about this, but the research shows that there are many pregnant women who did this and tragically had many birth defects come about in the process.
Bottom Line: The data is clear, iodine is toxic and these are not safe amounts worth advocating. In fact, they could be incredibly dangerous or even deadly.
4. Claim: Urine Challenge Tests Are Best For Evaluating Iodine Levels
When someone hears a claim that they need more iodine, or have an iodine deficiency more generally, they often want proof. Those in the Iodine Project base their recommendations on the results from a urine challenge test. In the test, a very high dose of iodine (normally around 50,000 mcg) is given. Following that, they have the patient collect their urine for 24 hours afterward. The thought is, if someone’s body has enough iodine, they will eliminate what they do not need. In truth, we do eliminate most iodine that is not needed through our urine. That is normal. However, the question is: when our iodine intake changes abruptly, how quickly does our urinary output reflect that change? The researchers here are assuming that, whatever you didn’t urinate out in a day, your body must have wanted or needed. But let’s unpack that a little bit more. If we think about an overt toxin, like mercury for instance, if someone took 2 mg of mercury and did not urinate it out in 24 hours, would that mean their body wanted the mercury?Key Insight: Urinary iodine levels take weeks and months to reflect changes in iodine intake.
This test was put to the test. A group of researchers had people do the test as advised but they kept collecting urine for days later. They wanted to see if all the iodine came out at once, or if it just took longer than 24 hours.21
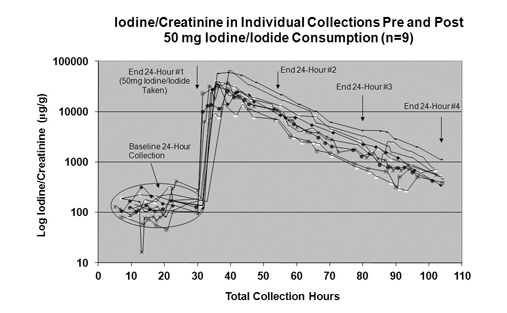
This chart essentially shows how much urinary iodine was present after the 24 hour period. The first thing you’ll notice, I’m sure, is that huge spike just outside of the 24 hours (around 30).
Simply put, the 24-hour test is simply not a valid tool. Many in this same group have also spoken about serum/blood tests, which are good for intense amounts of iodine toxicity, but are not useful simply in terms of tracking day-to-day iodine levels.
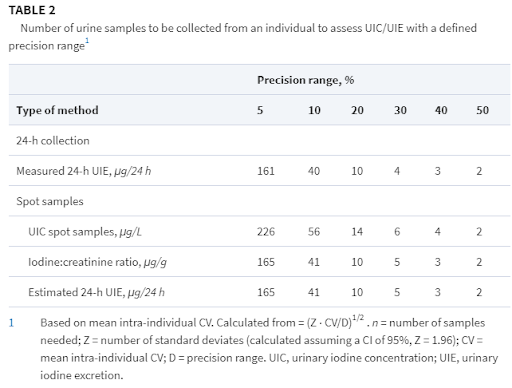
Urinary tests that do not involve challenge doses of iodine are useful to evaluate the iodine status of a population. Yet they have so much variability, they are not accurate for measuring any one individual.
In fact, you would need to repeat the test at least 10 times to be within even 20% of accuracy.22
The only time in all of the medical literature that an iodine challenge test was ever used was once in 1992. Researchers were checking to see how well people with kidney disease could eliminate iodine. They were given a challenge dose of iodine and their results were compared to those with normal kidney function. They eliminated less iodine in the following 24 hours than the control group. Yet the interpretation was not that they did so because they were iodine deficient, they did so because they had an impaired ability to regulate iodine.23
5. Claim: the Wolff Chaikoff Effect Isn’t Real
Researchers have observed since the 1940s that a high dose of iodine can stop the thyroid. Basically your thyroid has a safety switch. If too much iodine comes in, rather than make lethal amounts of thyroid hormone, your thyroid shuts off. It is a great example of homeostasis and has been used as a way to slow the thyroid when it is overactive.
Those in the Iodine Project argue that this mechanism is not real because its presence runs counter to their claim that megadose iodine helps the thyroid.
They argue that it is not real because of methodological problems with a 1948 study.
They argue that the rats in the study never became hypothyroid and thyroid hormones were not measured in their plasma.24
This misses the point of the study.
In fact, it was not done to see if the rats developed goiters or hypothyroidism. It was over too short of a timeframe for either to emerge. Neither of these conditions was discussed as topics of the study, nor were either of them measured.
Instead, they measured the rats’ thyroid function by removing and analyzing their thyroid glands directly. The speculation was that above some threshold of iodine, the gland would stop forming hormone despite the abundance of iodine. That is exactly what they observed.
The graph below shows that immediately after exposure to a high dose of iodine (plasma), the amount of thyroid hormones plummet.25 As plasma iodine drops, the thyroid hormones start to elevate again.
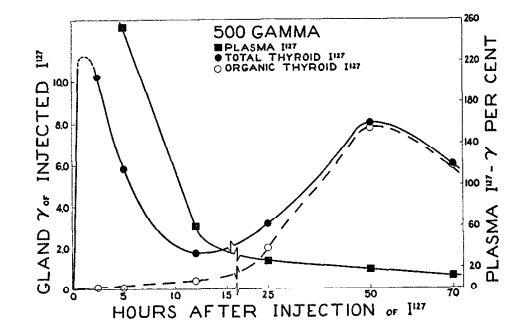
Prior to this period, iodine was used much more extensively in medicine than it is today. Doctors were observing that iodine could have negative effects on thyroid function. The more this issue was identified, the more doctors tried to find safer options.
This single study did not shift the tides against iodine. Doctors had commonly observed that high dose iodine could inhibit thyroid function.
This paper was not proving that the effect worked, it was exploring to find out how it happened.
The mechanism was even first observed in 1944.
At present we do not know if the effect can occur in anyone or only in those who are prone to thyroid disease. There are also issues about the finer points of the molecular mechanisms.
Overall, there has been no controversy about this mechanism since the Wolff-Chaikoff paper of 1948. Since then, we have learned:
- Many people do not get better from the Wolff-Chaikoff effect. They remain hypothyroid even after the high iodine exposure has stopped.
- The Wolff-Chaikoff effect can also trigger autoimmune thyroid disease — they are not separate.
- It is not all or nothing, because excess iodine in smaller amounts may slow the thyroid without fully stopping it.
- Some people can have the opposite effect, as high doses of iodine can trigger hyperthyroidism 26
How do we know it is real, though? It is because we have observed it in:
- Graves hyperthyroid storm
- Radioactive iodine prophylaxis
- Congenital hypothyroidism after maternal exposure to excessive iodine
In fact, some of the saddest stories involve the last point here. One study, titled “Congenital Hypothyroidism Caused by Excess Prenatal Maternal Iodine Ingestion” goes on to state:
“We report the cases of 3 infants with congenital hypothyroidism detected with the use of our newborn screening program, with evidence supporting excess maternal iodine ingestion (12.5 mg/d) as the etiology. Levels of whole blood iodine extracted from their newborn screening specimens were 10 times above mean control levels”27
The babies were born iodine toxic because the moms were taking it, and it shut off the baby’s thyroids. The Wolff-Chaikoff effect can also cause this to occur in babies when their mothers take too much iodine.
Sadly these are not the only such cases. There are other published case reports of this same condition arising after pregnant women were given iodine supplementation per the guidelines of the Iodine Project.28
Key Insight: The problem here is that the Iodine Project is stating that this is not a risk, when it clearly is. It is simply not safe to take as much iodine as they recommend.
We also know that this is relevant because of a medication known as Amiodarone. Essentially, 200 mg of this drug equates to 75 mg of iodine.
The average half-life is 58 days, meaning it takes 232 days to eliminate 92% of it. Most people on this medication have extremely high rates of developing thyroid disease.
We’ve also seen the effect in those with normal thyroid function and no thyroid disease. In Slovakia, people started developing endemic hypothyroidism as urinary iodine excretion elevated from 72 to 100, and finally to 513 mcg/g.29
We have also seen endemic goiter emerging in 64% of people in areas where children were exposed to similar amounts of iodine (in excess amounts).
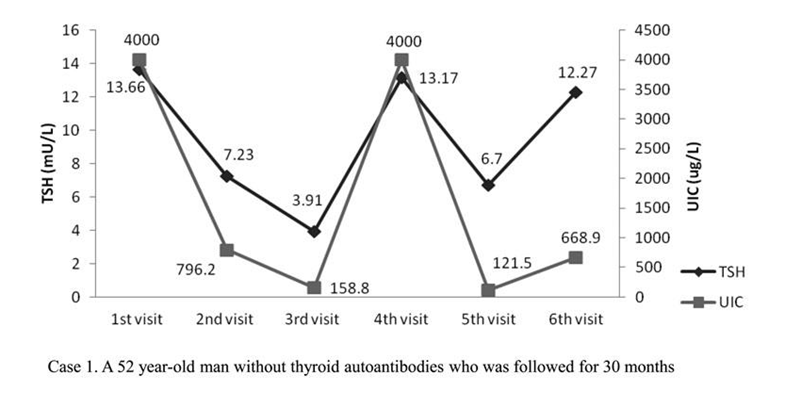
For some people, the effect that iodine has blocking the thyroid is incredibly predictable. The following chart shows both the TSH levels and the urinary iodine levels of a 52-year-old man. He was found to have subclinical hypothyroidism which was thought to be caused solely by his iodine intake.
This graph shows six separate readings each of his TSH and his iodine levels. A high TSH means an inactive thyroid. You can see how directly his thyroid slows as his iodine increases and vice versa.
Bottom Line: Just because a risk didn’t happen, does not mean it didn’t exist in the first place — or that it was a good idea. The same is true of iodine.
6. Claim: Halides Block The Effects Of Iodine
Halides, which are certain chemicals, can block the effects of iodine. That is the next big claim of the Iodine Project that I want to help break down for you.
In the Iodine Project, they argue that any possible apparent side effects from iodine are really effects from iodine pushing out halides from your body.
Fluoride
The one truth here is that fluoride is a halide, and it does compete with iodine for that sodium-iodide transporter. It keeps iodine from getting in by using up space.
Key Insight: Thankfully, the amounts of fluoride we are exposed to are far too low to have effects on thyroid function. We don’t get exposed in our day-to-day lives.30
Chlorine
Chlorine is another halide that many people talk about.
In the amounts that we are exposed to, from drinking water or swimming pools, chlorine does not affect our iodine metabolism.31,32
Bromine
The last important halide is bromine. Here is what we know from human studies:
One study looked at thyroid function in healthy people and compared it to urinary bromine levels. They concluded that there was no significant relationship between bromine levels and thyroid function, stating:
“The inhibitory effect of bromine is . . . compatible with the absence of detectable effects of a high intake of bromine on the thyroid gland”33
The other study was more useful since it checked more markers of human health, and because it gave bromine in doses much higher than what is typically ingested.
In a blinded human study, bromine in three doses was given to males and non-pregnant females for 12 weeks. The doses used were 0 (placebo), 4, or 9 mg of bromine per kg per day.
The normal daily intake is 2-8 mg per day total. For a 140 pound (63.6 kg) female, that would equal a range of 0.03 – 0.125 mg/kg per day.34
Key Insight: The active doses used in the study were up to 300 times higher than the normal intake of bromine.
No changes were observed for:
- T4
- Thyroid binding globulin
- Cortisol
- Estradiol
- Progesterone
- Testosterone
- TSH
- Prolactin
- LH
- FSH
There were also no changes in general blood chemistry or urinalysis.
One interesting finding was that women who were ingesting 300 times more bromine than normal had an increase in both T3 and T4 between the start to the end of the study.35
There is a point where we can get too much bromine, but it turns out there is also a point where we can get too little.
An iodine advocate stated: “There is no known therapeutic value for bromide. Therefore, any level of bromide could possibly cause problems.“36
Since the initial reports on bromine from the Iodine Project, we have learned that bromine is a nutrient essential to human life.
In 2014 it was named the 28th known essential element. Much of its roles involve collagen formation. Specifically, it is essential to forming Type IV collagen and sulfilimine.37
7. Iodine Does Cause High TSH (But It Is Not Relevant)
Here is a quick recap: TSH is a “backward marker” of your body’s overall thyroid hormone status. As it gets higher, your thyroid is more underactive.
Due to the W-C effect, many who take high amounts of iodine end up being hypothyroid. Those in the Iodine Project argue that, while it does happen, it is not important.
We know otherwise. TSH elevation is not a good thing, and it means that you are getting hypothyroid, the earliest sign of your body’s thyroid function slowing down.
- Ultimately, iodine exposure is known to cause
- Hypothyroidism
- Hyperthyroidism
- Goiter
- Autoimmune Thyroid Disease
- Nodules
- Thyroid cancer
- Fetal congenital hypothyroidism38
Other Claims Worth Mentioning
Above are some of the core claims made by the Iodine Project that I wanted to cover today. That said, I did want to dive into some secondary claims worth mentioning.
The following are some miscellaneous claims made by those in the Iodine Project that do not align with the basic sciences of human iodine metabolism.
Most of these points are used to support the general idea that massive amounts of iodine are helpful. They are as follows…
Claim: Iodide and Iodine Supplements Work Differently
Those in the Iodine Project have claimed that the different chemical forms of iodine (iodine and iodide) have distinct effects in the body. They have claimed that if someone had side effects from taking iodine, it was because they took it in a form with the ‘wrong ratios.’
The following image is an example:39
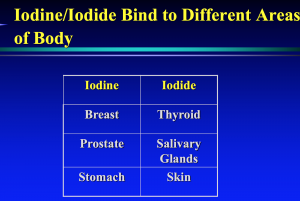
So, what is true about all of that? What we know is that, in food, iodine ends up being in the chemical form of iodide (as do iodine supplements).
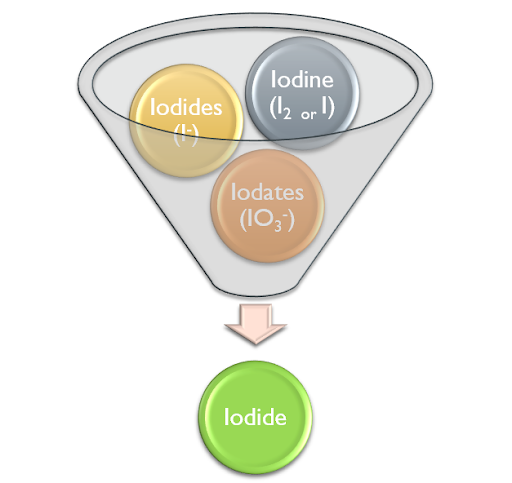
Even if you were to ingest iodine, your gut immediately turns it into iodide.40 This is also true when iodine is absorbed on the skin and it is why iodine can damage tissues that are trying to heal.
“Strong solution of iodine is corrosive and can cause blistering and necrosis of skin, commonly referred to as chemical burns or irritant contact dermatitis. Iodine has thus been replaced by substances known as iodophores that contain an iodine molecule linked to a large molecular-weight organic compound.”41
There is no iodine in circulation. The only place it exists in the human body is within the follicles of the thyroid gland. Even here it is a liability. When there is too much iodine, it damages the cells and triggers the inflammation that leads to autoimmunity.
How does this happen? There are four known mechanisms.
“(1) excess iodine induces the production of cytokines and chemokines that can recruit immunocompetent cells to the thyroid; (2) processing excess iodine in thyroid epithelial cells may result in elevated levels of oxidative stress, leading to harmful lipid oxidation and thyroid tissue injuries; and (3) iodine incorporation in the protein chain of thyroglobulin may augment the antigenicity of this molecule”42
Claim: The Body Stores Over 1,500,000 mcg (1.5 g) of Iodine
An iodine advocate argues the following:43
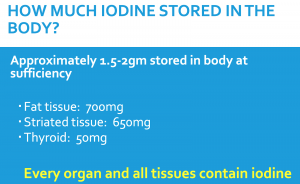
We know that, from radiographic analysis, that adults have about 15-20 mg of iodine in their whole body (most of which is in the thyroid)44.
With 70 – 80% in the thyroid, that means that outside the thyroid there will be no more than 6 mg of iodine.
Claim: Iodine Protects Against Breast Cancer
There is an argument that iodine is protective against breast cancer.
The logic on this is the observation that the Japanese have a higher iodine intake, and they have a lower rate of breast cancer.
If iodine were protective, and if the reason Japanese women have less breast cancer is because of their iodine exposure, we should be able to take them, look at their levels, and those with the highest iodine should have the lowest risk for breast cancer.
However, that has been studied, and the exact opposite was shown. It turns out that, across ethnicities, urinary levels of iodine are predictive for the presence of breast cancer45.
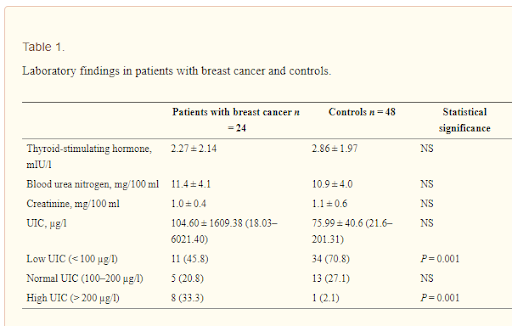
In the chart above you can see that women with breast cancer have much higher levels of iodine than those who do not.
Studies have shown that:
“iodine stimulated the transcriptional activity of estrogen receptor-α (ER-α) in breast cancer cells.”46
Researchers have talked about using urinary iodine as a screening tool to see who is at risk for breast cancer. Because iodine is associated with breast cancer, there is also research underway to see if radioactive iodine could be used to treat it.
Key Insight: There have even been discussions on whether or not iodine could be used as a tool to screen for breast cancer. Those who are highest are thought to be most at risk.
Claim: The Japanese Have High Iodine Intake and Good Health
While the Japanese may have better health, they do not have better thyroid function. It is not a coincidence that the first doctor to find the cause behind autoimmune thyroid disease was from Japan. That is why we call it Hashimoto’s Thyroiditis.
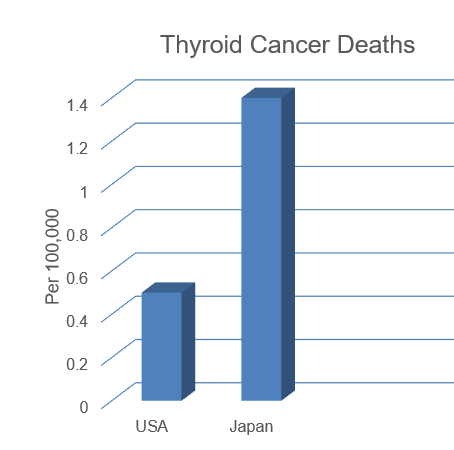
To this day, the Japanese have twice the rate of autoimmune thyroid disease as in the US.47,48 The Japanese also have three times the mortality rate, from thyroid cancer, as the US.49
In fact, After controlling for radiation exposure, the Japanese experience higher rates of all types of thyroid disease including,50,51
- Hypothyroidism
- Hyperthyroidism
- Subclinical hypothyroidism
- Subclinical hyperthyroidism
- Goiter
- Nodules
- Thyroid cancer
This high rate of thyroid disease is attributed to their high rate of iodine intake.
Claim: Iodine Makes Compounds Protecting The Body
A recent claim suggests that there is something iodolactone, which is where iodine forms lipid proteins that protect the thyroid.52
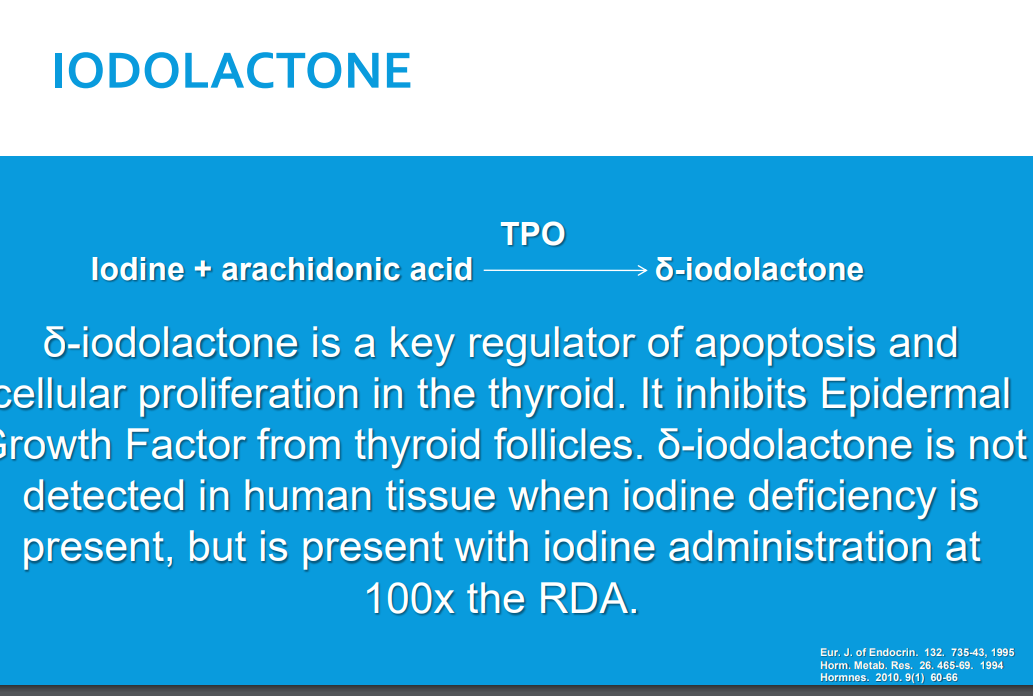
Iodolactone is known to be produced by mice when exposed to high doses of iodine and arachidonic acid.
None of the studies cited here or in other works were on humans. In test tubes, iodolactone is formed when an inflammatory chemical called arachidonic acid is oxidized in the presence of iodine.
In humans, iodolactone was measured once. It was found in a single patient with Graves disease who had her thyroid shut down by high dose iodine.53
We have no evidence that iodolactone is present in humans or is clinically relevant in humans.54
Key Insight: What we do have is strong evidence that iodine is the main trigger of thyroid suppression and autoimmunity in cases of autoimmune thyroid disease.55,56
How Can They Make These Claims?
If you make a claim that is contrary to nearly all of the world’s biomedical literature, it would demand robust amounts of evidence.
The first step would be tracking outcomes in a peer-reviewed case review paper. This is hard to claim when there are numerous published case reports of complications from high dose iodine supplementation.
The Iodine Project: Summarized
Ultimately, I don’t want to question anyone’s sincerity or intentions.
That said, I see a lot of this research as being influenced heavily by confirmation bias. This means relying on data that only proves your point, and ignoring everything else.
This mistake was all generated by assuming that the symptomatic improvements in fibrocystic breast disease were from the nutritional role of iodine, not its pharmacologic effects.
In short, I think it is okay to let go of these ideas and embrace what we know based on data and good research. So, let’s talk about what we can do starting today…
The Big Points
Here’s everything you need to know about the Iodine Project and iodine today in the world:- Iodine is not good or bad. We need some, but too much is harmful.
- Is iodine deficiency truly a thing? Most people in the modern world have enough iodine. Some who have or are prone to thyroid disease are at risk for too much iodine.
- Severe iodine deficiency no longer exists on planet earth.
- Iodine can be toxic — in fact, it was once a leading cause of suicide.
- The Wolff Chaikoff effect is real, and it relied on every day in medicine.
- Halides do not block iodine.
- Urine challenge tests are not accurate.
- There are no perfect tests.
- Iodine can cause high TSH and other symptoms — these are relevant changes
What Can You Do?
Here are some action steps you can take today:
- Iodine is safe for most humans at a range of 50 – 200 mcg/day or 150 – 250 mcg/day for pregnant/nursing women
- Those who do not have and are not prone to thyroid disease can occasionally tolerate higher doses
- Regulating iodine can reverse Hashi, Hypo, and SCH. The levels that do this is 50 – 100 mcg per day57,58,59
Finding the best Data
Thank you so much for sticking with me today to learn more about the Iodine Project, and everything you need to know about this incredibly important topic.
In the end, I want to help you operate on good data, and make decisions that truly benefit your life while circumventing some pretty obvious (and potentially harmful) risks.
Feeling ready to get started? I’d love for you to take Iodine Intake Calculator (Click Here: Take The Quiz Today) today. It can help you build on what we’ve talked about today, and create a true roadmap for better health in the future.
Resources