Let’s talk about testing your adrenals.
Here’s a quick introduction to the concept of adrenal testing. If you have unexplained symptoms, like feeling wiped out, faint, bouts of insomnia, poor stress tolerance, or anxiety, it is worth it to screen your adrenal function.
There are many ways it can affect your overall health, and lifestyle can make a big difference. The first step is as simple as taking the Adrenal Quiz (Click Here: Take the quiz today)
Past that point, the best testing would be a combination of:
- Blood markers (for morning cortisol), and
- ACTH and DHEA
- Salivary tests (for both morning and nighttime cortisol)
Product Recommendation: Are you at a heightened state at all hours of the day for no particular reason? The Stressed Pack can lower your cortisol. Click Here for the Adrenal Health Pack – Stressed
Contents
hide
Explaining ‘Adrenal Fatigue’
This is a concept I went into detail with when I was writing the Adrenal Reset Diet. Let’s start by addressing this idea that has created a big rift in medicine: adrenal fatigue. The conventional world says that it is silly, there is no evidence behind it, while the natural world says it is real and it gets better through supplements1.It’s tough because these groups are talking past one another. But, there is a faulty premise behind the idea of ‘adrenal fatigue’ (Read More: Why I want to rename adrenal fatigue).
The argument is that someone’s cortisol is low, because the adrenals are worn out and unable to make more2.
Addison’s Disease
It’s plausible, but the circumstances are a bit different. There is a rarer disease called Addison’s disease, and this is one example of where the adrenals are fatigued because the body has beat them up (through damage caused by the immune system). The thing is that these low levels of cortisol can be identical in both adrenal fatigue and Addison’s disease, but the difference is in what the body is trying to do. What we can do to solve for that is by measuring the brain signal that is telling the adrenals what to do.Key Insight: It’s called ACTH, and it is equivalent to what TSH is to your thyroid. It is your brain telling your adrenals to work.
In the case of Addison’s disease, where the adrenals are just broken down, ACTH is high. The body is trying to get the adrenals to work and make more cortisol, but they simply can’t keep up. In the case of adrenal fatigue, both cortisol and ACTH are low (low-normal or low below range).
The Truth About Adrenal Fatigue
In the case of adrenal fatigue, cortisol levels are low because the body simply wants a break from cortisol. The body is run down, there have been real problems from chronic stress, and there are a number of other factors that could be at play here, too.All that said, what the body needs is to not be stimulated. It needs to rest and recover. So, while it is a real thing, it is not what we might call or term ‘adrenal fatigue’ (Read More: The top three myths concerning adrenal fatigue).
Adrenal Stress
In short, the adrenals are not weak or fatigued. It’s rather that the whole system is dysfunctional and not being regulated properly. So, if we could, I’d love to change the name. For the rest of today’s article, let’s use the term ‘adrenal stress.’Bottom Line: By the last count, there have been approximately 8,000 studies uncovering the realities of hypothalamic pituitary adrenal dysfunction, so it is a real thing!
Adrenal Symptoms Leading To Disease Risks
‘Adrenal fatigue’ is real, while not aptly named. We know that the symptoms involved can lead to some consequential disease risks for many. This could include:- Chronic inflammatory states
- Immune abnormalities
- Cancers
- Bodyweight changes
- Chronic depression, anxiety, and mental health symptoms
Understanding Adrenal Slopes
One of the more dramatic examples of this entire idea of adrenal stress is known as the Whitehall II study. This was done on a group of British civil servants, between 2002 and 2006, with a large range of adults involved3. What the researchers were doing was tracking all the various health metrics, including their ‘cortisol slope.’ So, let’s start by expanding on this idea. When it comes to cortisol, we should make a lot of it in the morning and shut it off at night. If you plot those two lines together, you get a very clever slope (like a ski slope, from up to down). They have shown that the cortisol slope is independent of how much cortisol you have. So, it’s not just about whether you have enough, but if you have the right slope. This could mean you have normal amounts, but it’s the same all day, or if it is backward, or if it is always low. In this sense, it’s not bad because of the amounts, but because of the pattern of those amounts. Even the best amounts, when they don’t slope, can have a negative effect.Breaking Down The Study
In this previously mentioned study, they were checking a variety of health metrics, like:- Weight
- Blood pressure
- Cholesterol
- Blood pressure
- Smoking status
Cortisol Slope: 4 Distinct States
We start with an understanding of our cortisol slope, how important it is, and then we need to dig a bit deeper into the different ways it can reveal itself. Here is the breakdown:- Level 0: Thriving
- Level 1: Stressed
- Level 2: Wired & Tired
- Level 3: Crashed
Thriving
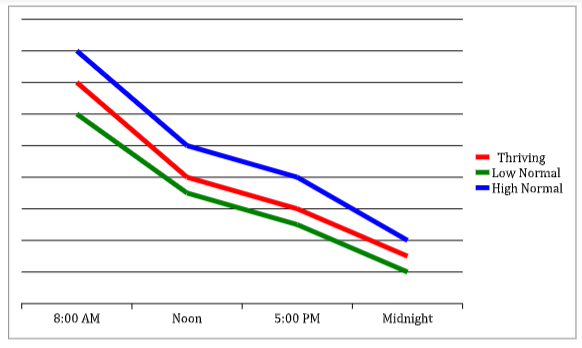
This is when you have your cortisol high in the morning, low in the evening, and your cortisol slope is looking good. There is some normal range for fluctuation, but on the whole things are looking quite normal in this stage.
Stressed
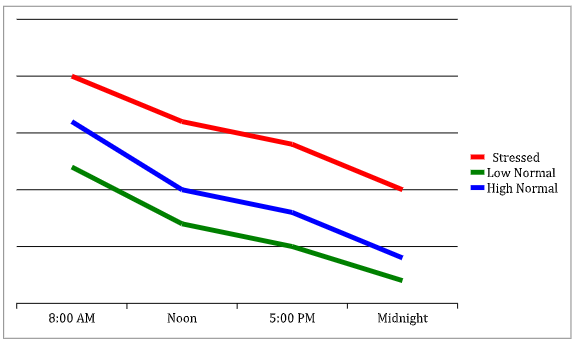
Here is where things like your chronic stress response begin to set in. Your slope is always a bit higher than it should be, and it is an indication that things are starting to go a bit awry and your body is ‘stressed’ as a result.
Wired & Tired
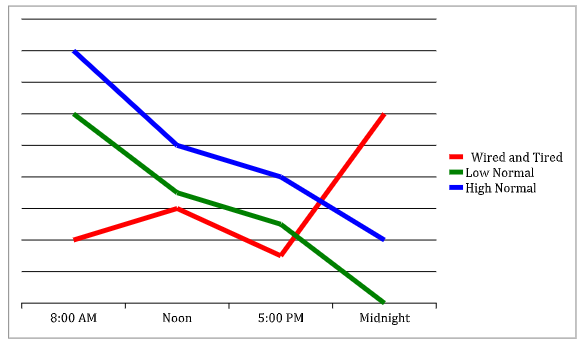
The easiest way to think about this stage is in the form of a backward slope. Your slope has become flipped: it’s lower in the morning, and higher at night.
Crashed
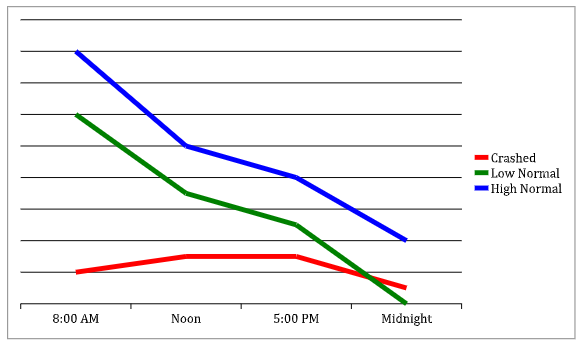
This is where things are always low, and it’s less of a slope and more of a flat line. This is where things have effectively ‘crashed.’
How Does This Unfold?
There have been some debates as to whether these things can unfold in a step-by-step fashion. Someone can have adrenal stress, and maybe they won’t start right away in stage one and move in a linear fashion. Maybe, instead, they will kick things off in stage three. So, the sequence is not set in stone, but the examples provided are all examples of poor cortisol slope and are proven predictors of pretty bad health consequences. And, they are also things that can be diagnosed in quite a straightforward fashion. But, how do we do that?Diagnosing Adrenal Disease Versus Dysfunction
Let’s start with diagnosing adrenal diseases.- Addison’s disease is the most common, which causes the adrenals to much too little hormone, but there are some that cause the glands to make too much, which could include:
- Tumors on the adrenals
- Congenital adrenal hyperplasia
- Then, we also have Cushing’s disease. This is where there is excess cortisol from taking it or from the body making too much of it.
- Lastly, we have pheochromocytoma. That is a situation where there is tissue, much like adrenal tissue, but it is not where it’s supposed to be.
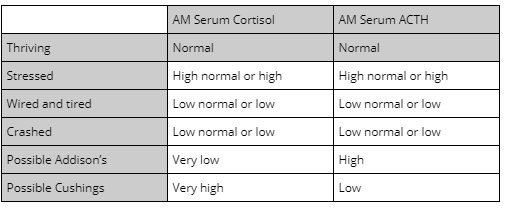
Key Insight: You can easily make sense of all these by simply looking at your serum cortisol patterns from your blood (as well as serum ACTH patterns).
It is common to simply look at your cortisol levels, and nothing else. But, by looking at ACTH, you can tell the difference.
Here is a quick table to make sense of it all…
Should You Test Your Adrenals?
So, how do you know when you should be testing your adrenals? The first step should be when you’re dealing with symptoms that you just can’t explain. This might include:- Fatigue
- Slow metabolism
- Depression
- Blood pressure (too low or too high)
- Postural orthostatic tachycardia syndrome (a drop in blood pressure when standing)
What Kinds of Adrenal Tests Work Best?
Let’s break down each kind of test and some of the key advantages, and disadvantages, of them…Adrenal Blood Tests
These can offer you immediate hormone levels, while testing some important markers like cortisol, ACTH, and DHEA sulphate. Sometimes, though, serum tests may have variability based on movement and short-term stress levels.Hair Tests
Hair tests are general tests that have a longer-term average of 3-8 weeks. They are also not clinically available, and presently only used for research purposes4.Salivary Tests
Salivary cortisol tests are accurate and helpful for evaluating cortisol slope. That said, it is not as accurate for other important markers like DHEA5.Urinary Tests
A 24-hour urine test can be a good tool to show daily total production, but it fails to show circadian patterns. Dried urine is also not as helpful for circadian patterns, but overall urinary tests are reasonably accurate for morning and midday cortisol (but not so much in the evening)6.What Are The Best Adrenal Levels?
Once you have the data you need, based on the above tests, what levels are the best for you? Here’s a big table to help you make sense of it:| Test (units) | Time | Low | Optimal | High | |
| Blood tests | Cortisol | 6-8 AM | < 5 mcg/dL | 10 – 20 mcg/dL | >25 mcg/dL |
| ACTH | 6-8 AM | 7.2 pg/mL | 9.5 – 36.7 pg/mL 4 | 63 pg/mL | |
| DHEA-S 5Female 30-39 | 6-8 AM | 45 µg/d | µg/d | 270 µg/d | |
| DHEA-S 6Female 40-49 | 6-8 AM | 32 µg/d | µg/d | 240 µg/d | |
| DHEA-S 7 Female 50-59 | 6-8 AM | 26 µg/d | µg/d | 200 µg/d | |
| DHEA-S 8Male 30-39 | 6-8 AM | 120 µg/d | µg/d | 520 µg/d | |
| DHEA-S 9 Male 40-49 | 6-8 AM | 95 µg/d | µg/d | 530 µg/d | |
| DHEA-S 10Male 50-59 | 6-8 AM | 70 µg/d | µg/d | 310 µg/d | |
| Salivary tests (units and normal ranges can vary per lab) | AM Cortisol | 6-8 AM | 13 nM | same | 24 nM |
| Noon Cortisol | 11 AM – 1 PM | 5 nM | same | 10 nM | |
| Afternoon Cortisol | 4 – 5 PM | 3 nM | same | 8 nM | |
| Nighttime Cortisol | 10 – Midnight | 1 nM | same | 4 nM | |
| DHEA-S | 6-8 AM | 3 ng/mL | same | 10 ng/mL |
What Do You Do If Things Aren’t Normal?
The main thing you need to know is that it can be fixed! I have talked about it before (Read More: The Science Behind Adrenal Stress), but the thing to note is that diseases have various treatments, as does dysfunction. In fact, you can even fix it promptly. We even see that someone can go from having the worst levels, to the best levels, in the span of only a few months. That’s a huge change, and relatively speaking it can happen so fast. The general ideas are, though:- Getting enough light exposure in the morning (a half-hour of sun)
- Having quality protein first thing in the morning (22 or more grams)
- You want some good, healthy carbs with your evening meal
- Reverse light exposure with a good hour’s break of light
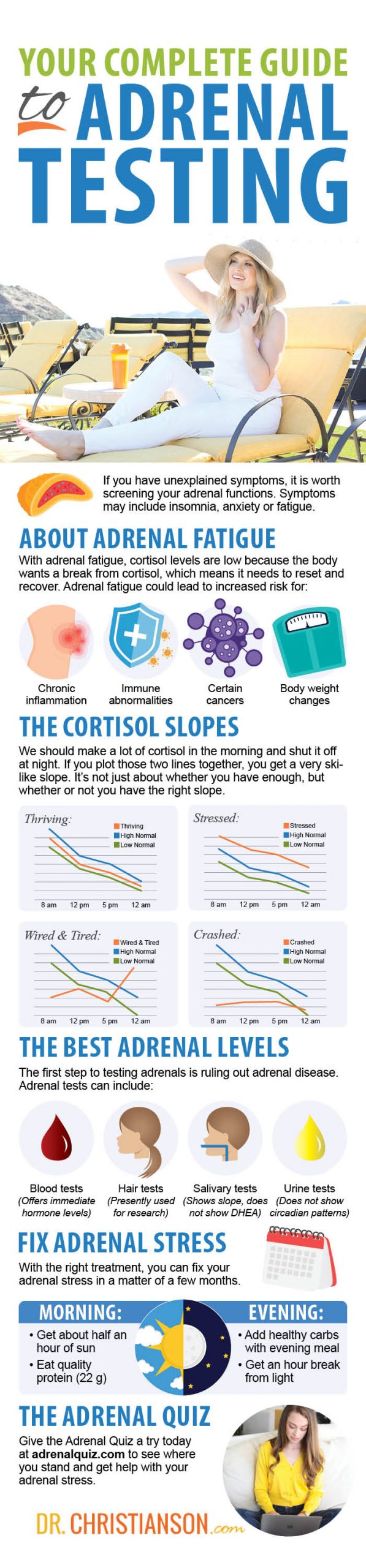
Try The Adrenal Quiz Today
Again, I can’t help but stress the importance of giving the Adrenal Quiz a try (Click Here: Give it a shot right now!). It can really give you a great sense of where you stand, and some of the steps you can take to help with adrenal stress. I hope you’ll give it a try right now.Resources
1 – Cadegiani FA, Kater CE. Adrenal fatigue does not exist: a systematic review [published correction appears in BMC Endocr Disord. 2016 Nov 16;16(1):63]. BMC Endocr Disord. 2016;16(1):48. Published 2016 Aug 24. doi:10.1186/s12902-016-0128-4
2 – Powell DJ, Liossi C, Moss-Morris R, Schlotz W. Unstimulated cortisol secretory activity in everyday life and its relationship with fatigue and chronic fatigue syndrome: a systematic review and subset meta-analysis. Psychoneuroendocrinology. 2013;38(11):2405-2422. doi:10.1016/j.psyneuen.2013.07.004
3 – 1. Adam EK, Quinn ME, Tavernier R, Mcquillan MT, Dahlke KA, Gilbert KE. Diurnal Cortisol Slopes and Mental and Physical Health Outcomes:A Systematic Review and Meta-analysis HHS Public Access. Psychoneuroendocrinology. 2017;83:25-41. doi:10.1016/j.psyneuen.2017.05.018
4 – Wester VL, van Rossum EF. Clinical applications of cortisol measurements in hair. Eur J Endocrinol. 2015;173(4):M1-M10. doi:10.1530/EJE-15-0313
5 – Ceccato F, Barbot M, Zilio M, et al. Performance of salivary cortisol in the diagnosis of Cushing’s syndrome, adrenal incidentaloma, and adrenal insufficiency. Eur J Endocrinol. 2013;169(1):31-36. Published 2013 Jun 1. doi:10.1530/EJE-13-0159
6 – Sakihara S, Kageyama K, Oki Y, et al. Evaluation of plasma, salivary, and urinary cortisol levels for diagnosis of Cushing’s syndrome. Endocr J. 2010;57(4):331-337. doi:10.1507/endocrj.k09e-340
P.S. Whenever you are ready, here is how I can help you now:
1. Schedule a Thyroid Second Opinion with me, Dr. C, Click Here for Details
2. Download and use my Favorite Recipes Cookbook Here
3. Check out my podcast Medical Myths, Legends, and Fairytales Here
Dr. Alan Glen Christianson (Dr. C) is a Naturopathic Endocrinologist and the author of The NY Times bestselling Adrenal Reset Diet, The Metabolism Reset Diet and The Thyroid Reset Diet.
Dr. C’s gift for figuring out what really works has helped hundreds of thousands of people reverse thyroid disease, lose weight, diabetes, and regain energy. Learn more about the surprising story that started his quest.



